Individuals with and without migraine share a fundamental need for meaningful experiences and deep connection. While these ideals may be attainable to the status quo, people with migraine may be deprived of these core needs due to the stigma surrounding migraine.
Support, validation, and feelings of purpose and contentment strengthen our identity to self and community. Without these basic needs, becoming empowered and visible members of society becomes a goal, not a reality.
What is Stigma?
Stigma refers to the harmful labeling, stereotypes, biases, judgements, and prejudices that become attached to a certain group of people based on a diagnosis or trait, and in this case, migraine.1 8 It is a socially and culturally informed process, fueled by the constructs, values, and beliefs given at a specific place in time.
Migraine: A Stigmatized Disease
Contrary to public perception, migraine is a major public health issue with extensive impacts, both personal and economic.
- One billion people worldwide have migraine.1
- Migraine costs $30 billion a year in healthcare costs and productivity.1
- In 2016, migraine was the second leading cause of global disability and neurological disease burden.2
Migraine is real, migraine is pervasive, and the people who have migraine matter.
Underrecognized, Underfunded, and Misunderstood
Despite these realities, the world at large remains tethered to false, outdated, and sexist perceptions of migraine, complacently allowing further stigma to ensue. As a result, stigma has extensively infiltrated and dictated migraine recognition, diagnosis, and treatment.3 4 5
Consequently, people with migraine are commonly subjected to societal disproval and discrimination. They may be forced to navigate environments unwilling to accommodate their needs which are deemed insignificant. This lack of visibility and validation spoils identity, leaving those with migraine with marred personhoods and diminished social connections. In conjunction with the trivialization of migraine that occurs within social systems, medicine, and legislation, it is widely reported that migraine is underrecognized, underfunded, and misunderstood.2 5 8
Measuring Migraine Stigma
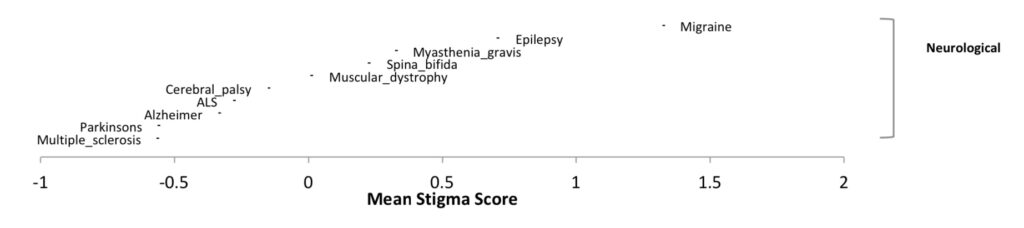
The Stigma Scale for Chronic Illness (SSCI) is used to assess stigma among people living with chronic illnesses. Utilizing this assessment, chronic migraine was shown to have more stigma than epilepsy, which had a score similar to that of episodic migraine.20 25
Did You Know?
Ability to work was shown to be an indicator of stigma in migraine—increased work-related disability correlates with stigma for people with chronic migraine.20
Types of Stigma
Migraine does not exist in a vacuum. At the interface of migraine and society exists stigma.8
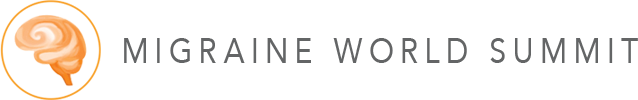
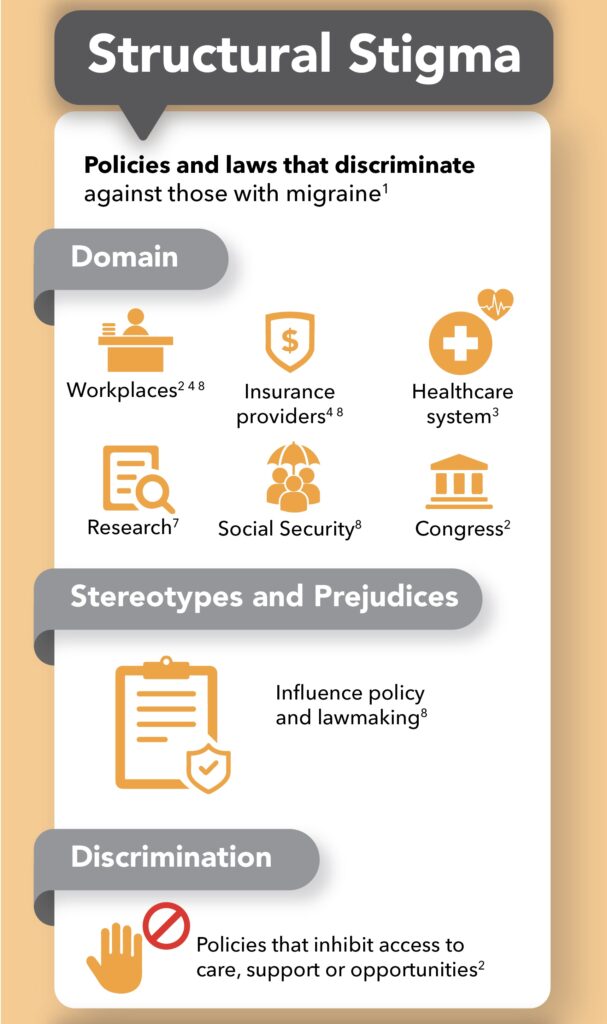
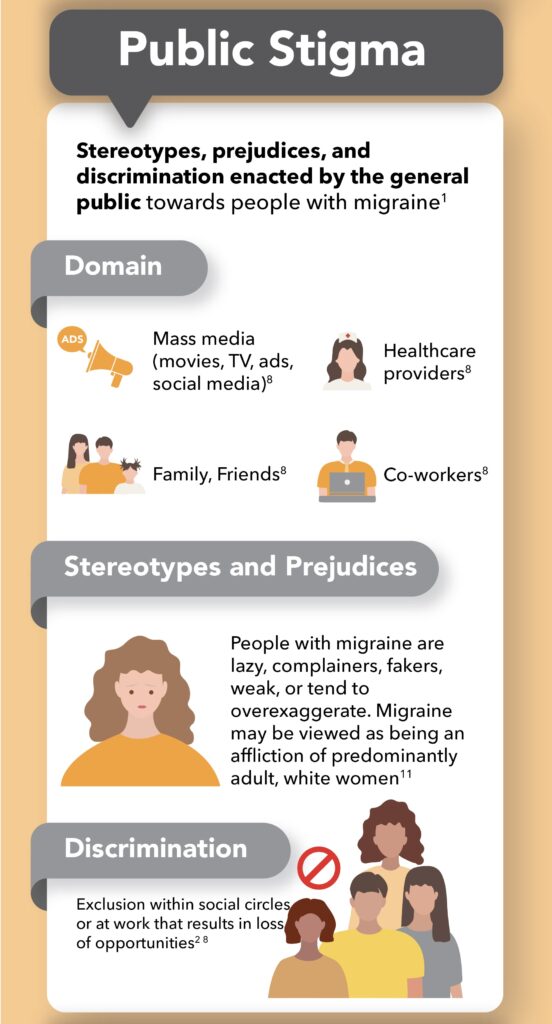
Layered over time and filtered through cultural lenses, stigma permeates society, and influences our thoughts, feelings, and actions. Due to its pervasive nature, there are three types of stigma:1
- Structural stigma
- Public stigma
- Self-stigma
Summary
What is Migraine Stigma?
Stigma refers to the harmful labeling and negative biases that are attached to a certain group of people based on a trait or diagnosis, in this case migraine. Despite migraine being an established debilitating, neurological disease that has profound personal and economic impacts, stigma has infiltrated perception, awareness, and treatment.
Migraine stigma has deleterious effects on quality of life, policy making, and accessibility to treatment.
Stigma can be broken down into three categories: structural, public, and self-stigma.
Structural stigma refers to the policies and laws that discriminate against people with migraine, while public stigma is the stereotypes and prejudices enacted by the general public. When those with migraine internalize and perceive the prejudices and negative biases they’ve experienced to be true, self-stigma results.
Contributing Factors of Stigma in Migraine
Marginalization and Dismissal
Migraine is an equal opportunity disease—all ages, ethnicities, abilities, and socioeconomic classes can have migraine. However, due to racial disparities and lack of access to care, migraine disproportionately affects more Black, Indigenous, and People of Color (BIPOC) as compared to white people. Despite this, BIPOC are often excluded from research and discouraged from seeking help.7
Racism
Minorities’ pain is often not validated or respected. The notion that BIPOC can tolerate pain better than white people can be traced back to slavery. Minimization and suppression of pain was expected when being auctioned, as smiling through physical abuse made slaves more auctionable. This psychology still exists within the healthcare system, and BIPOC are more likely to be stigmatized.7
Cultural Differences
Cultural scripts can dictate acceptable expressions and communication of pain. Some cultures value stoicism and encourage silence when experiencing pain. The resulting cultural dissonance between patient and physician increases the likelihood of dismissal and stigma.7
Validity of Migraine as an Invisible Illness
Migraine is an invisible illness on two levels:
- It cannot be seen by others.1 2
- Labs or scans cannot provide proof of its existence amongst patients.1 2
Symptom-Based Diagnosis
Diagnosis of migraine is symptom-based and dependent upon patient evaluation. Neuroimaging or biomarkers cannot confirm a diagnosis, and though it is disabling, migraine’s invisible nature often leads others to disregard it as a valid disability. 8 As a result, many fail to validate its presence, and assume those with it must be fakers. 9
Denial of Migraine
The denial of migraine as a legitimate disease is central to the stigmatization of migraine.2 Without tests to justify migraine’s impacts, patients become responsible for providing the “proof”. As a result, migraine’s validity falls on the character of patients, and specifically their character flaws.10
Blaming Migraine on Character Flaws
Because migraine is viewed as a minor personal issue rather than a legitimate disease, the people with migraine are often judged as having character flaws which are to blame for their affliction.11 The dialogue therefore shifts from a framework of disease to one of blame, influenced by stereotypes and misinformation.10 11 18
Stereotypes and Misinformation
Negative stereotypes of migraine discredit the reality of the disease and the challenges faced by those experiencing it.
Common stereotypes attached to people with migraine and the resulting statements made include:¹¹
- Lazy
- “What an easy life you have staying in bed all day.”
- Complainers
- “When I don’t feel good, I still go to work. It’s what you do.”
- “Stop complaining, you should just be grateful.”
- “It could be worse.”
- Overly sensitive or weak
- “You’re just too sensitive, you need to toughen up.”
- “Why can’t you just do [insert activity]? It’s not that hard.”
- “Well, you still have to do [insert activity].”
- Drug seekers incapable of coping with pain
- “If you can work, it must not be that bad.”
- Fakers who overexaggerate
- “That’s your excuse for everything.”
- Neurotic and excessive worriers
- “Mind over matter, right?”
In addition, online representations often depict migraine as an “annoyance.” Google searches of migraine show adults, mainly women, simply touching their heads and wincing in pain. This depiction is rarely the reality, and it reinforces inaccurate stereotypes that minimize migraine.²
Other media representations use migraine as a metaphor for devaluation, comparing annoyances or stressful events to being a “migraine” or “headache”.²
Gendering Migraine
The genderization of migraine has contributed to its delegitimization and subsequent stigma. In the past, historical narratives and pharmaceutical advertisements have contributed to sexist attitudes towards migraine, downplaying its severity and placing blame on the individual experiencing migraine.¹¹
Historical Perspective
Migraine stigma has changed throughout the centuries, reflecting the beliefs, attitudes, and values of society.
Throughout the 16th- and mid-17th century, migraine was treated as a legitimate disease, bolstering its existence within the medical sphere and garnering compassion and effective treatments (for that time period).¹²
During the 18th and 19th centuries, public perception of migraine transformed to a more gendered illness, one experienced primarily by poor, exhausted women, and scientific and intellectual men.¹²
This transformation from legitimate disease to minor affliction continued into the 20th century, which ushered in the rise of “migraine personality.” This “type A” personality categorized migraine as a character flaw held by highly sensitive, elite women (often housewives) who overthink and worry excessively.¹¹
Freud even postulated women’s uncontrolled impulses were to blame for migraine attacks. Consequently, those with migraine were treated as being hysterical, and the doctors who treated them “enablers”.5
Role of Pharmaceutical Industry
The “Typical Migraine Patient”
When marketing migraine treatments, some pharmaceutical companies have portrayed the typical migraine patient as a white, privileged, professional, upper-middle class woman with children. Specifically, these advertisements emphasize this woman’s inability to care for her children during a migraine attack.¹¹
Misrepresentation
While this scenario may ring true for some, it is not the epitome of, nor does it do justice to, the migraine experience.
By fixating on white women as the primary target, i.e., gendering migraine, the pharmaceutical industry has unilaterally misrepresented the migraine community, both in identity and experience. Marginalization of BIPOC and lower-income patients reinforce the notion that migraine only afflicts white women of a certain class. This exclusion and biased perception perpetuates stigma and discrimination.¹¹
Silence Perpetuates Stigma
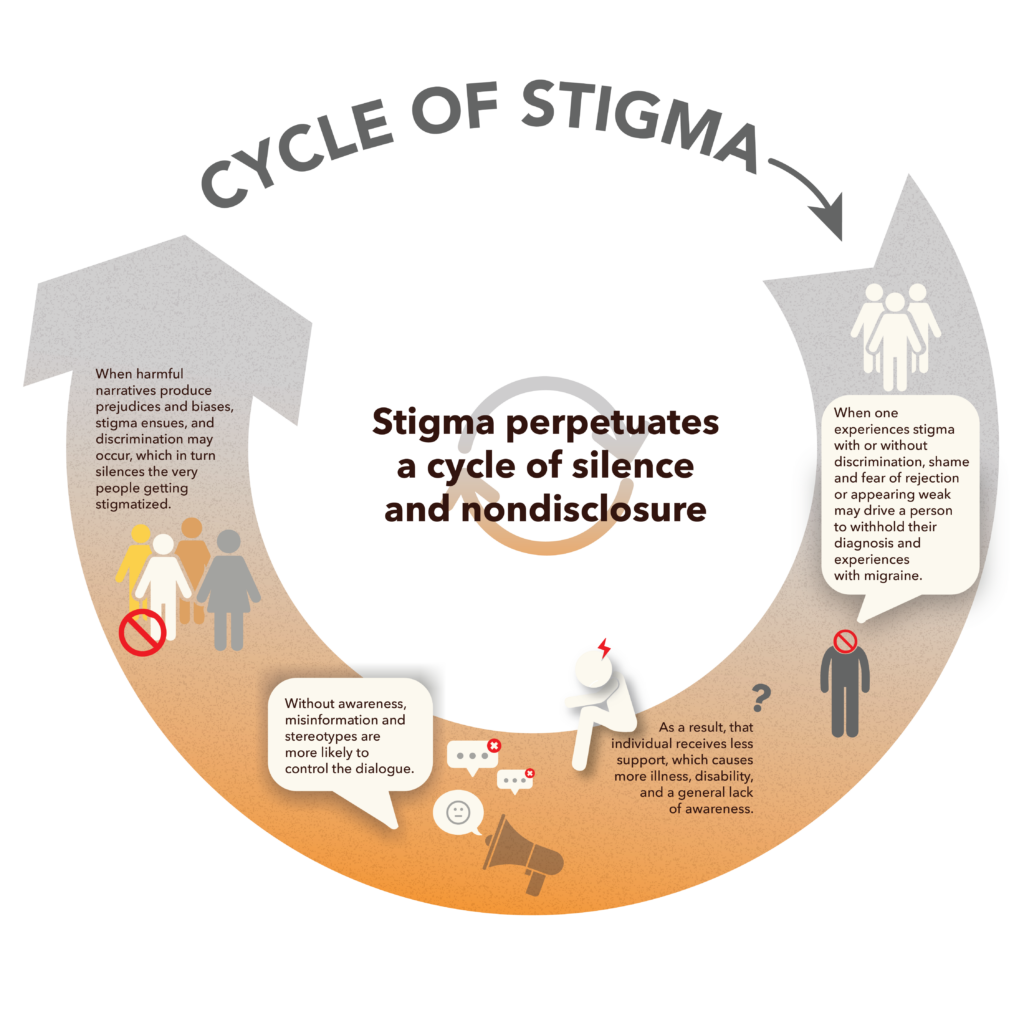
When faced with structural, public and self-stigma, nondisclosure is the unfortunate consequence experienced by many.¹³ While this silence may be an impact of stigma, it is also a cause, yielding a Catch-22 situation.
Summary
What Causes Migraine Stigma?
Migraine stigma is caused by a variety of factors, all of which are tied together by dismissal and a lack of validity.
Because migraine is an invisible illness and diagnosis is symptom-based, many do not view migraine as a legitimate disability. Blaming migraine on perceived character flaws (being neurotic, weak, lazy, overly sensitive) compounds this issue of denial and reinforces negative stereotypes.
Misrepresentation in the media (such as pharmaceutical ads) excludes BIPOC, who often experience dismissal due to racism and cultural barriers.
Fear of rejection and shame may prevent people with migraine from speaking up, and the silence and nondisclosure that result further perpetuates stigma.
Impacts of Migraine Stigma
Increased Disability
Psychological Distress and Nondisclosure
Stigma Silences
Self-stigma negatively affects self-esteem and mood, and triggers a hiding reflex in individuals with migraine so as not to expose the parts of themselves of which they feel ashamed.1 14
Guilt, self-blame, and fear of rejection compound these feelings and discourage individuals with migraine from speaking out, resulting in silence and nondisclosure.4 10 13 14
Isolation
When enacted, stigma devalues and isolates those with migraine.8 Exclusion within social circles has negative impacts on individuals who are already forced to retreat due to repeated migraine attacks.
The subsequent discomfort with being one’s true self depletes energy and increases disability.11
Lack of Visibility and Validation
People with vaginas are often not believed or heard when sharing their experiences with migraine, and this contributes to the lack of visibility and validation experienced by people with migraine.15 16
Worsening of Migraine
Due to self-stigma, some people with migraine may not feel comfortable seeking a diagnosis or treatment. As a result, migraine may worsen.3
Delays in Treatment
On average, it takes 18 months to receive a correct diagnosis. Within this time frame, upwards of $12,000 may be spent in health care costs, not including work-related expenses.3
Incorrect diagnoses and inappropriate medications make treating migraine more difficult. Without support, migraine may worsen, as delays in treatment make migraine harder to manage.3
Cultural Barriers
In addition, cultural barriers may affect the relationship between physician and patient, making it more difficult for BIPOC to feel connected and heard within the healthcare system. Consequently, trust becomes harder to build, and BIPOC experience obstacles in receiving diagnosis and treatment.7
Structural Inequities
Workplace Discrimination
Did You Know?
A diagnosis of migraine colors the professional opinions of employers—4 out of 5 employers thought migraine was an invalid reason to call out from work.8
Lost Jobs and Increased Employer Costs
Ninety percent of people with migraine cannot continue working during an attack, and the remaining 10% who do continue are only half as productive.10
Without appropriate accommodations and support in the workplace, people with migraine may experience a worsening of migraine or may need to quit altogether.10
Both possibilities are costly to employers, whether it be through increased health care costs, or an increased need for recruiting, training, and hiring—all of which decrease morale and productivity.10
Did You Know?
Thirty four percent of individuals with migraine have experienced discrimination or hardships at work due to stigma.21
Legislative Gaps
Underfunded
Stigmatized disorders receive less funding than non-stigmatized disorders. Consequently, migraine receives a fraction of research funding relative to its impact in disability adjusted life years (DALYs). DALYs are a measure of disease burden assessing years of life lost due to disability and mortality.2 11
Comparatively, arthritis, breast cancer, and digestive diseases all have similar DALYs as migraine. As of 2015, these diseases received appropriate funding relative to their impact: $214 million, $674 million, and $1.6 billion, respectively. Migraine, on the other hand, only received $20 million.2
Limited Research
Without proper funding, less research can be conducted, and without research new medications cannot be developed.2
Fewer clinicians may view migraine research as a successful career option, limiting the number of research scientists advancing migraine care, which further shunts migraine awareness.2 8
Barriers to Care
Lack of Specialists
Due to a lack of available research grants, medical students and residents may feel hesitant entering a field with slim prospects of a successful career.2
As a result, there are fewer than 700 certified headache specialists available to treat the 55 million Americans with migraine.26
This lack of appeal is even exchanged amongst established physicians, who may view headache medicine with condescension, holding a “courtesy stigma” towards the physicians who treat migraine.2
Furthermore, without adequate funding, publicly funded laboratories, which invent two-thirds of new migraine medications, are not able to discover new medications.2
Did You Know?
Medical students generally only receive a few hours of education in headache medicine. Exposure to headache cases often does not occur until clinical training, most likely in the third or fourth year.22
Coverage Impediments
Structural stigma discriminates against people with migraine through unfair policies, causing coverage impediments.2
For instance, receiving medication or treatment can be more difficult for people with migraine due to unfair insurance policies governing migraine.4
In addition, there is currently no listing for migraine in Social Security’s Blue Book, despite being the second leading cause of global disability. As a result, applying for Social Security disability benefits is more difficult for people with migraine.2 8
Did You Know?
Migraine has existed for centuries, but criteria for diagnosis didn’t exist until 1989.3
Lastly, employers may not acknowledge migraine’s severity and impact, impeding the process of applying for worker’s compensation.2
Summary
What Are the Impacts of Migraine Stigma?
Individuals with migraine exposed to stigma may experience increased disability and psychological distress. Shame and isolation may prevent people with migraine from speaking up and seeking treatment, which can worsen migraine.
Structural stigma results in structural inequities. Workplace discrimination and a lack of accommodations put individuals with migraine and employers at risk for lost jobs and increased costs. Lack of research funding and specialists in the headache field limit the development of new medications and treatments, and unfair policies create coverage impediments and barriers to care.
Combating Stigma in Migraine
Advocacy
Due to stigma’s silencing effects, advocacy necessitates courage. 1 8 11 Effective advocacy is rooted in empathy and is patient, not pharmacy, led.11 14 18
Disclosure
Disclosure within healthcare settings helps establish an honest relationship between patient and doctor, and transparency aids physicians in choosing the most appropriate treatment for each patient. 4
Likewise, disclosure at work benefits the person with migraine in the following ways:
- It makes employers aware of migraine.10
- It gives employers the opportunity to provide accommodations.10
- It allows employers to be more understanding of any migraine related absences.10
Language
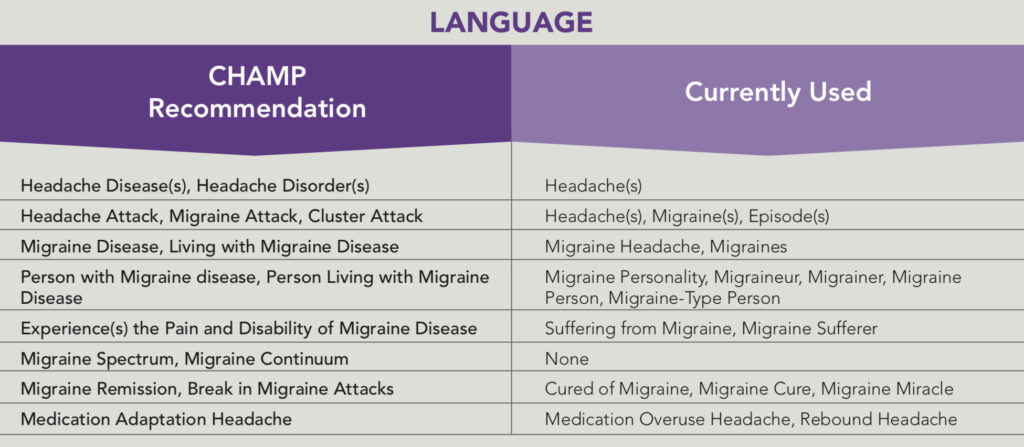
In order to stamp out migraine stigma, we must change the language used to describe it.10
Validating the Person with Migraine
Appropriate language should acknowledge people with migraine as human beings first and foremost. Extracting migraine from personhood to reveal and celebrate the humanness of each person with migraine will lay a foundation of basic human dignity and respect.11 18
Validating Migraine as a Disease
Language chosen that will acknowledge and validate migraine as a legitimate disease is fundamental to breaking the stigma.2 The Coalition of Headache and Migraine Patients (CHAMP) offers the following guide to facilitate validation through language:24
Education
In order to become better advocates, people with migraine and their supporters must understand the disease. Educating yourself and others allows us to build more effective and articulate dialogue.4 14 18
One avenue worth considering is social media, which offers a substantial influx of information and support. It facilitates a sense of community and growth, and online support groups establish camaraderie among fellow migraine patients.17
Reframing Migraine
People with Migraine
In order to establish migraine as a legitimate disease, those with it must be acknowledged appropriately. Common labels circulating society devalue and isolate those with migraine. A new script is needed—one that validates the true experience of migraine and acknowledges those with migraine as strong and heroic.6 One with migraine could be likened to a warrior—a “migraine warrior”—i.e., strong individuals who display bravery and perseverance in the face of disabling disease.
Furthermore, people with migraine can rewrite their own perception of their experience. Relinquishing self-blame and guilt allows the individual with migraine to embrace compassion and acceptance for themselves and others with migraine.6
Physicians
Sharing how migraine impacts a patient’s life takes tremendous courage and authenticity, especially when instances like these may have been met with disbelief and invalidation in the past.11
Doctors should be sensitive to the lifetime of stigma their migraine patients may have endured. Listening and believing that their pain is real will help reframe physician’s perception of migraine, which will help break the stigma.11
Pharmaceutical Industry
The pharmaceutical industry strongly influences migraine perception through medication advertisements.11
Advertisements highlighting the diversity within the migraine community, as well as the spectrum of impacts people with migraine face will assist in reframing migraine.11
Likewise, a more realistic portrayal of the lived experience of migraine can help guide others in viewing migraine with a more compassionate and understanding lens. Doing so will allow people with migraine to be their authentic selves.11
Legislative Action
Receiving increased visibility from government entities combats stigma by establishing migraine as a legitimate disease worthy of federal government attention.8
In order to boost migraine visibility at the structural level, Congress must allocate more funds to the National Institutes of Health (NIH) for migraine research. By doing so, headache medicine will garner more interest from doctors and researchers, which will grant people with migraine better access to care.2 11 As a result, migraine will have a greater presence in medical curricula, and neurology departments will seek more headache specialists.2 11
Summary
Combating Migraine Stigma
Advocacy is key. Patient participation and community involvement can challenge stigma and reframe migraine as a legitimate disease worthy of visibility, validation, and federal government investment.
Speaking up and educating others increases awareness and challenges stereotypes and misconceptions. Mindfully choosing language that validates both migraine warriors and the disease itself will garner more respect, compassion, and empathy for the migraine community.
Legislative action and policy reform will provide increased structural support in the form of research and medications.
Looking Ahead: Destigmatizing Migraine
Advocacy in the Community
Those with migraine who are comfortable advocating can begin in smaller settings amongst family, friends, neighbors, and coworkers. Doing so will increase visibility in social circles, and others will be more apt to offer validation.18
Helpful tips to keep in mind include:
- Honesty and openness: Self-advocacy can be as simple as sharing how one truly feels when asked “how are you?” By honoring and expressing your needs, it helps others to understand migraine’s impacts. Sugarcoating a true experience in order to avoid discomfort may mislead the general public and strip those with migraine of social support.18
- Have resources available to share with others: Unfortunately, honest expressions may fall on disbelieving ears. In these cases it’s helpful to have a list of websites available to assist others in understanding migraine disease.16
- Non-combative and non-accusatory: It’s especially important to steer any justified emotional reactions toward advocacy. Remaining objective and non-accusatory will help communicate messages more clearly. By creating a welcoming and nonjudgmental space for others it allows them to reevaluate their biases and preconceived notions.11
Self-advocacy can be frightening, especially when past attempts have been disregarded. Not feeling ready or able to advocate is completely valid and should be honored.11
Advocacy at Work
Gaining accommodations in the workplace simultaneously acknowledges migraine’s impacts and increases productivity.10
Key points to keep in mind when disclosing migraine to employers:
- Disclosure in writing is preferred.10
- Disclose as soon as possible.10
- Keep documentation of what was exchanged between employer and employee, as well as dates.10
- Informing employers of any known triggers and/or worsening of migraine attacks will help maintain transparency.10
- Provide a doctor’s letter or medical records to aid this process.10
Advocacy in the Government
The United States Federal Government is the largest funder of biomedical research in the world.11 Members of Congress are responsible for the allocation of funds to the NIH, who in turn fund public research laboratories.2 19
Lobbying members of Congress to allocate more funds for migraine research will allow public research laboratories to perform more research and discover new migraine treatments.2
Bottom Line
Stigma is a serious problem with significant personal and structural impacts. To the detriment of the migraine community, stigma has warped public perception of migraine with sour representations and negative associations, discrediting both the experiences and identities of individuals with migraine.
Despite these impacts, stigma can be addressed and challenged through advocacy and patient mobilization strategies. Speaking up and raising awareness is key to affecting communal and legislative change. With proper research funds and increased visibility and validation, destigmatizing migraine is possible.
FAQs