Nestled between sleep and wakefulness, a morning headache is a common occurrence among people with and without migraine. This painful and unwelcome experience uncovers sleep’s role in migraine, and simultaneously, migraine’s effects on sleep. Though this relationship may not be clear as day, creating an action plan to combat a morning headache is both accessible and effective.
Why You May Wake Up with a Headache
1. Poor Sleep Habits
Poor sleep habits can impact both the quality and duration of sleep. Common traps that could induce an early morning headache include:
- Not managing stress: Tension, either from tight muscles, anxiety, or an improper sleep position can trigger an early morning headache. Similarly, teeth grinding or clenching can also contribute to facial or head pain.1
- Under- or oversleeping: Both scenarios can disrupt the body’s natural sleep-wake cycle, resulting in an early morning headache.
- Irregular sleep schedule: Whether erratic sleep is due to jet lag, shift work, or the weekend “catch-up”, inconsistent sleep can disrupt the circadian rhythms and impact the production and release of melatonin, a hormone responsible for inducing sleep.1,4
- Electronic use: The blue light emitted from electronics interferes with the body’s natural release of melatonin, a sleep-inducing hormone.2
“Patients who don’t sleep well over time have trouble with pain control. So the less we sleep, the more likely we are to have pain.”1
2. Sleep Disorders
All sleep disorders constitute some level of decreased sleep quality or duration.
- Sleep apnea: Marked by gaps in breathing, sleep apnea can affect oxygen levels. If a morning headache lessens as oxygenation levels improve throughout the course of the day, sleep apnea may be the culprit.1
- Insomnia: Lack of sleep or delayed sleep can trigger migraine or tension-type headache.4
- Restless leg syndrome: Movement during sleep can impact sleep quality and contribute to a decreased pain threshold and morning headache.1
- Sleep bruxism: Clenching the jaw or teeth grinding can increase muscle tension in the facial and head region, increasing the likelihood of a morning headache.1
3. Circadian Rhythm Disorders
Circadian rhythm disorders refer to disturbances in the circadian rhythm, or internal biological clock. When this system is out of sync with the environment, sleep and other biological processes are impacted.5 Decreased alertness, daytime sleepiness, or a morning headache can all be caused by a circadian rhythm disorder.
4. Headache Disorders
- Migraine: Migraine attacks can be triggered by poor sleep quality and inconsistent sleep schedules. Additionally, people with migraine may experience poor sleep prior to a migraine attack. This may be due to spikes in serotonin levels during the night, causing fragmented sleep.2
- Medication Overuse Headache: When over-the-counter pain relievers or prescription headache medications are used too frequently or for too long, a nighttime withdrawal could result in a morning headache.1
- Hypnic Headache: Hypnic headache is a prime example of a dysregulated sleep-wake pattern. Characterized by attacks that awaken someone from sleep at the same time each night, this type of headache often begins in middle age and can last from 30 minutes to 6 hours.6
- Cluster Headache: This type of headache is marked by severe pain in or around the eye or on one side of the head, congestion, excessive tearing or redness of the eye, and restlessness. Attacks can be cyclic and awaken someone from sleep.7 Excess sleep is a reported trigger for cluster headache.4
Did You Know?
While many with migraine may experience poor sleep as a trigger, it could actually be part of the prodrome, or the first phase of migraine. In other words, your migraine attack may be triggering poor sleep, not the other way around.1
5. Mental Disorders
- Depression and Anxiety: Common among individuals with migraine, depression and anxiety are often accompanied by physical symptoms, such as appetite changes, sleep disturbances, or headache.9
- Maladaptive Behavioral Patterns: If mornings become synonymous with head pain, consider evaluating any mental health factors that may be preventing a restorative and deep night’s sleep. For example, catastrophizing and hypervigilance, common behavioral patterns seen in people with migraine, may cause unease throughout the day and before bedtime.9,10 As a result, if you aren’t able to wind down your body and mind, sleep could be impacted.
6. Other Medical Disorders
- Intracranial Hypotension: If a morning headache occurs upon standing up, but is absent when lying down, intracranial hypotension could be playing a role. This type of headache is caused by low levels of cerebrospinal fluid, which cushion the brain and spinal cord. Without adequate cushioning, compensation occurs, causing vasodilation and increased pressure in pain-sensitive areas.11
- Brain Tumor: Awakening from sleep with head pain in no way points to a brain tumor. However, if a severe headache in the morning is accompanied by other symptoms indicative of a brain tumor, speak to your doctor.12
7. Hormonal Factors
- Female Sex Hormones: Fluctuating hormone levels are a common migraine trigger. In fact, hormones are believed to be a contributing factor in the three-fold higher prevalence of migraine among people with vaginas than those with penises. If you are experiencing morning head pain around menstruation, hormones may be a likely cause.13
- Melatonin: Produced in the pineal gland, melatonin is a hormone that induces sleep. Studies show melatonin levels may be low in people with chronic migraine.8 Consequently, lower than normal levels of melatonin can negatively impact sleep quality and duration, causing an increased risk of an early morning headache.
8. Lifestyle Factors
Similar to sleep habits, these daytime habits can have a direct impact on sleep:
- not staying well-hydrated
- skipping meals or eating a large meal before bed
- consuming caffeine past noon, or caffeine withdrawal
- alcohol consumption
9. Environmental Factors
- Allergens: Dysfunction of the autonomic nervous system, which controls involuntary processes, links migraine and allergies. Allergen-induced inflammation triggers congestion, sneezing, fatigue, and headache.14 Additionally, the release of histamine causes dilated blood vessels and a rise in nitric oxide levels, which is associated with migraine attacks.15
- Mold: Mycotoxins, which are present in mold spores and released into the air, can cause headache, fatigue, or difficulty concentrating. While more research is needed in this area, bedrooms with mold may play a role in a morning headache.16
- Chemicals: Sensory sensitivities are hallmarks of migraine disease. Synthetic fragrances or other chemicals found in some perfumes, air fresheners, or body products can trigger migraine. If you’re sleeping in a room with a triggering chemical or scent, it could be causing a morning headache.
10. Medications
- Sleeping pills: Studies show that certain sleep medications can actually worsen headache.1 Talk to your healthcare professional for medical advice if you think a sleep medication may be causing a morning headache.
- Overusing pain medication: Taking prescription or over-the-counter painkiller medication too frequently can cause medication overuse headache, which may be experienced upon awakening.1
Summary
Reasons Why You May Wake Up with a Headache
Common causes of morning headache may include issues related to:
sleep habits, including unmanaged stress, under or oversleeping, inconsistent sleep/wake times, or electronic use before bed
sleep disorders, circadian rhythm disorders, headache disorders, mental disorders, or other health conditions
lifestyle, hormonal, and environmental factors
medications
Treating Migraine and Comorbid Sleep Disorders
While a morning headache may respond to over-the-counter medications, such as acetaminophen or ibuprofen, embracing a holistic approach can promote wellness and prevent future morning attacks.
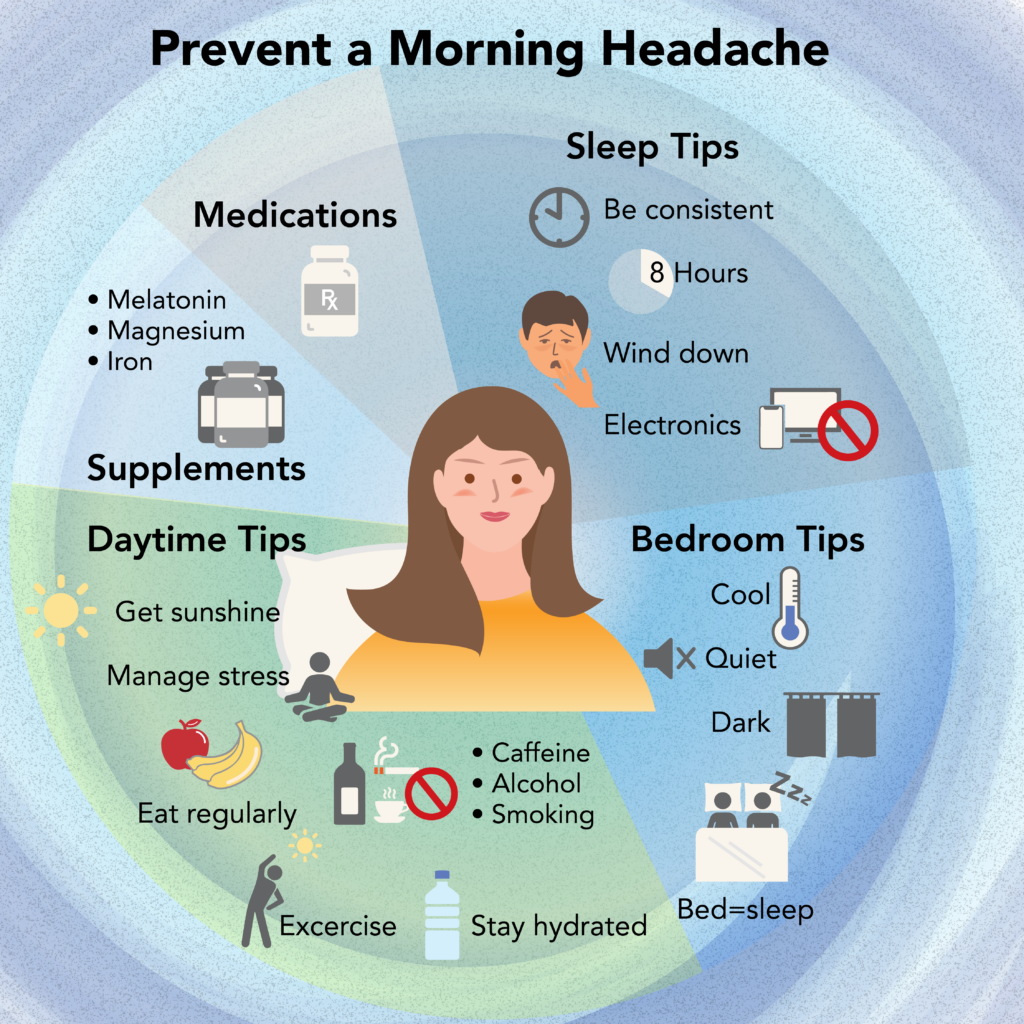
Sleep Hygiene
“The most common [sleep disorder] really is just poor sleep hygiene. A third of us are guilty of that.”2
Sleep hygiene refers to the healthy habits, behaviors, and environmental conditions that aid in achieving quality sleep. Incorporating sleep-friendly practices and avoiding sleep-disrupting activities is key for migraine and sleep disorder treatment.
Start a Sleep Routine
- Sleep schedule: Strive for regular and consistent sleep patterns, i.e., wake up and fall asleep at around the same time each day.
- Sleep duration: Adults should aim for eight hours of sleep each night, while children and teens need eight and a half to ten hours of sleep.
- Wind down time: Set aside time to wind down before bed, and include relaxing activities, such as meditation. Dimming the lights can also help cue the body for sleep.
- Electronics: Avoid using electronic devices before bed, as the blue light emitted from electronics inhibits the release of melatonin. If complete elimination is not realistic, you can use the “night mode” function to reduce blue light and prepare the brain for sleep.
Did You Know?
Studies show that people who meditate before bed have enhanced melatonin levels, slow-wave (deep) sleep, and rapid eye movement (R.E.M.) sleep.17,18
Optimize Bedroom Conditions
- Cool temperatures: Keep the bedroom between 65 and 68 degrees Fahrenheit, and avoid dressing too warmly.
- Quiet environment: Use a sound machine if noise is an issue.
- Dark bedroom: Use shades or blackout curtains to prevent light from peeking through windows.
Key Point
How fast should I fall asleep?
Ideally, sleep onset should occur after 20 minutes of being in bed. Rapid sleep onset may be a sign of sleep deprivation or exhaustion, while delayed sleep onset could indicate various issues pertaining to sleep hygiene or a sleep disorder.1
Lifestyle Changes
As you optimize sleep hygiene, consider exploring how daytime habits may be impacting sleep.
- Sunlight: Get your daily dose of sunshine to help keep the circadian rhythm functioning as nature intended.
- Stress management: Reduce stress through meditation, deep breathing, talk therapy, or social support. If temporomandibular joint (TMJ) disorder or teeth grinding is present, talk to your doctor about using a mouth guard.
- Diet: Eat regularly to keep steady blood sugar levels, and avoid a large meal before bed.
- Hydration: Stay well-hydrated throughout the day, and avoid drinking too much water right before bed.
- Caffeine and alcohol: Avoid caffeinated beverages past noon, and limit alcohol consumption.
- Smoking: Don’t smoke—nicotine disrupts sleep, and smoking is a risk factor for snoring and sleep apnea.19
- Exercise: Strive for daily sweat-inducing movement, but avoid exercising within two hours of bedtime.
- Bedroom activities: Only use the bedroom for sleep or sex.
- Napping: While a nap can help fight a migraine attack, it can also disrupt the circadian rhythm and cause more sleep problems. If you need to nap, limit them to no more than 30 minutes, or consider going to bed earlier.
Cognitive Behavioral Therapy for Insomnia
Cognitive behavioral therapy for insomnia (CBTI) is a first-line treatment option for people with insomnia. Drawing from cognitive behavioral therapy, CBTI explores the underlying behavioral issues that may be perpetuating sleep deprivation. It focuses on two facets: stimulus control and sleep restriction.1
- Stimulus control addresses any environmental stimuli that could be preventing sleep onset and continuity.
- Sleep restriction aims to eliminate nighttime awakenings by restricting the time spent in bed. For example, if someone is in bed for ten hours but only sleeps for five and a half hours, then their time in bed would be restricted to six hours. This process will repeat, until over time, their time spent in bed parallels their time spent sleeping.
Key Point
Treat Sleep Apnea
Sleep apnea causes snoring, pauses in breathing, and daytime sleepiness. It also causes drops in oxygen levels throughout the night, making treatment especially important. If you think you may have sleep apnea, seek a sleep specialist to obtain a sleep study. Treatment often includes a CPAP (continuous positive airway pressure) machine to help keep the airways open for better oxygenation and better sleep.
Supplements
Widely available and generally cost-effective, supplements can be a relatively simple addition to your migraine toolbox.
- Melatonin: Naturally produced in the brain, melatonin prompts sleepiness, aids in relaxation, and reduces alertness. Studies show that people with chronic migraine have lower than normal levels of melatonin.8 Taking 3 mg of melatonin may help raise levels and decrease migraine attacks.20
- Magnesium: Magnesium is a critical mineral that aids in relaxation, stress reduction, and sleep. Magnesium deficiencies, which 50% of people with migraine have, can cause irritability, insomnia, tension headache, or migraine attacks.21,22 While this supplement can be taken in various forms, 400 mg in pill form is a great place to start.21
- Iron: Ferritin is a protein that stores iron and releases it as needed. Low ferritin levels could indicate an iron deficiency and is a common cause of restless leg syndrome.1 If you experience this sleep disorder, speak to a healthcare professional about the possible benefits of an iron supplement.
Medications
Sometimes poor sleep and increased migraine attacks may require pharmacological intervention. In these cases, adding a sleep medication can help break that cycle and offer an emotionally corrective experience.
Zolpidem (Ambien) and eszopiclone (Lunesta) are commonly used for insomnia. These medications have less habituation and less tolerance than benzodiazepines. In addition, usually, the same dose can be taken for longer periods of time.2
Summary
Treating Migraine and Comorbid Sleep Disorders
Treatment options for migraine and comorbid sleep disorders include behavioral intervention, supplements, and medications.
For better sleep, start a sleep routine that incorporates sleep-friendly habits:
– Keep the bedroom dark, cool, and quiet, and avoid working where you sleep.
– Aim for 8 hours of sleep every night.
– Wind down before bed by meditating and limiting electronic devices.
Be mindful of how daytime habits may affect sleep:
– Get sunshine.
– Manage stress.
– Eat regularly and stay hydrated.
– Limit caffeine and alcohol, and don’t smoke.
– Exercise no later than 2 hours before bed.
– Keep the bedroom for sleep or sex.
For those with insomnia, cognitive behavioral therapy for insomnia is a first-line treatment.
Additionally, supplements, such as melatonin, magnesium, or iron can aid in sleep. In some cases, medication may be necessary to break a poor sleep and migraine cycle.
Bottom Line
Due to sleep’s highly impactful nature, there are numerous reasons why someone may wake up in the morning with a headache. Issues related to sleep, medical conditions, or lifestyle factors could be possible causes of a morning headache.
Improving sleep quality and consistency is key to the successful treatment of migraine and comorbid sleep disorders. Through behavioral intervention, supplements, and medications, a morning headache can be addressed, treated, and prevented.
FAQ Section
Additional Resources
- Snore Lab app records and tracks snoring
- Migraine Buddy helps track migraine symptoms and triggers


