Good sleep is hard to come by, and not just for people with migraine—approximately 80% of the world has some form of sleep disorder.1 The impacts of this global sleep deficit are widespread and extend beyond migraine, affecting cardiovascular and metabolic health.
For people with migraine, sleep is especially powerful. Whether it’s acting as a symptom, trigger, or treatment for an attack, sleep’s role in migraine management is undeniable. Further, the sleep difficulties associated with migraine can impact disease progression, development of comorbid conditions, and quality of life.1,2,3
The Relationship Between Migraine and Sleep
Bidirectionality
“Pain interferes with our ability to fall asleep and stay asleep, but not getting enough sleep or having that circadian misalignment actually makes pain worse.”3
Sleep and migraine are inextricably linked, and changes to one can impact the other. In the throes of a migraine attack, sleep can feel like a tall order, and understandably so. In a similar light, after a poor night’s sleep, a migraine attack may be just around the corner. This cycle not only interferes with successful migraine treatment outcomes, but it can also create additional health problems.1
Studies show that a high migraine frequency correlates with poor sleep quality.4 This relationship isn’t causal, but bidirectional: People with migraine are more likely to develop a sleep disorder than the general population, and vice versa.2
Sleep Disorders Comorbid with Migraine
At first glance, migraine and sleep disorders may seem like two categorically distinct subsets of illnesses. Each is ideally treated by different specialists—migraine by a headache specialist and sleep disorders by a sleep specialist. Despite this, both headache and sleep quality are tightly linked issues affecting many people.
Did You Know?
Individuals with migraine are two to eight times more likely to have a sleep disorder than those without migraine.3
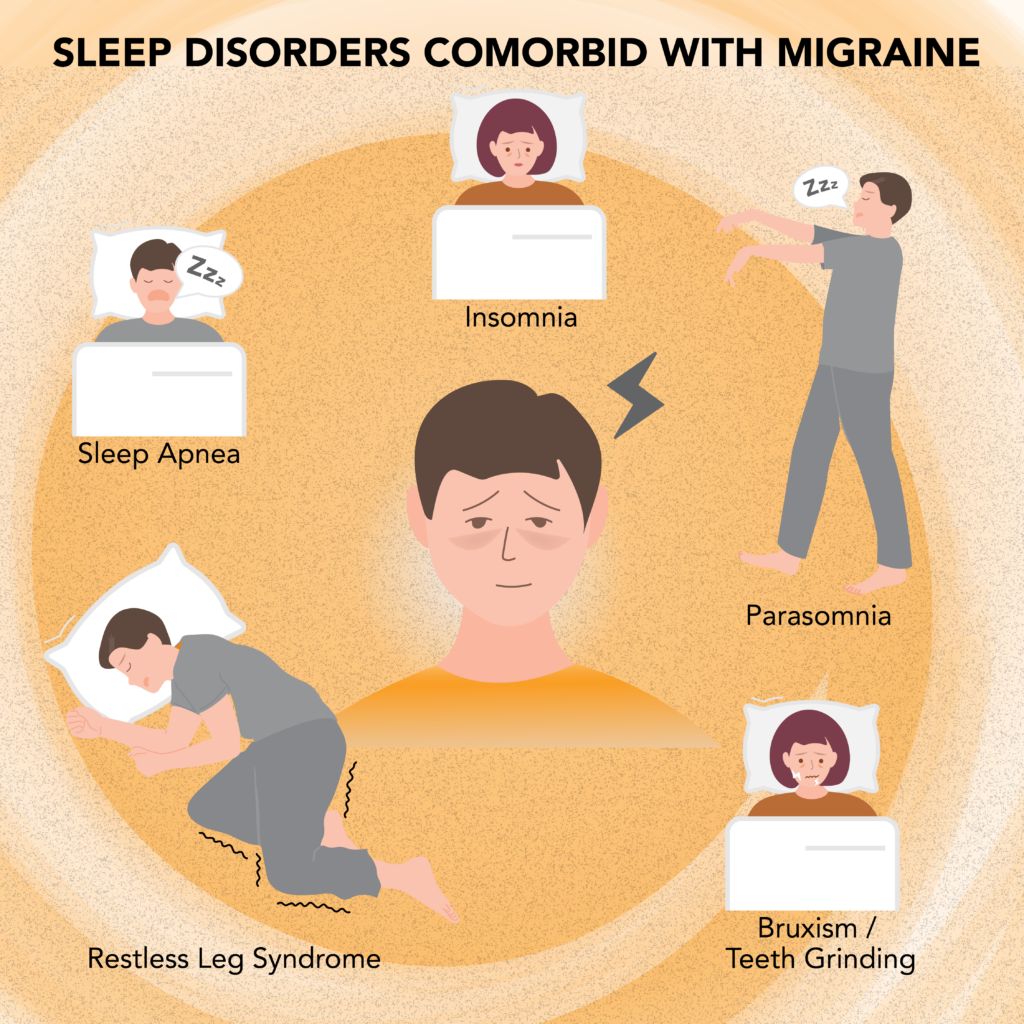
Sleep Apnea
Sleep apnea’s well-known symptom, loud and continuous snoring, is not the only sign of this potentially serious condition. Pauses in breathing, mouth breathing, daytime sleepiness, and a morning headache also mark this sleep disorder.2
Common among men, sleep apnea causes drops in oxygen levels, as well as concerns for cardiovascular and liver function.5
Insomnia and Parasomnia
Insomnia, which is twice as common in people with migraine than those without, refers to difficulty falling or staying asleep.3 Insufficient sleep from insomnia can have profound impacts on general health, especially when left untreated for years. In addition to migraine, tension headache is particularly impacted by insomnia.4
Another sleep disorder that is comorbid with migraine are parasomnias, such as night terrors and sleepwalking.4 Parasomnias can occur during any stage of sleep and interfere with sleep continuity.6
Bruxism
Sleep bruxism, or teeth grinding, is a sleep-related movement disorder. Common among people with migraine, bruxism can be due to stress and can affect the TMJ (temporomandibular joint).1 Treating bruxism may require a mouth guard to protect your teeth.
Restless Leg Syndrome
In restless leg syndrome, people will have an uncontrollable urge to move their legs during the day or night.8 While the causes are unknown, it could be due to genetic variants, low levels of a protein called ferritin, or dysfunction in the part of the brain responsible for movement.1,7
Summary
Migraine and Sleep
Migraine and sleep share a bidirectional relationship, i.e., having one disorder increases the chance of developing the other disorder. This can create a maladaptive cycle, where pain triggers restless sleep, and poor sleep incites a morning headache.
Migraine is comorbid with certain sleep disorders, including sleep apnea, insomnia, parasomnia, bruxism, and restless leg syndrome. These conditions interfere with sleep quality and increase the risk of an early morning headache.
How Sleep Affects Migraine
Whether you’re sleeping peacefully or tossing and turning all night, sleep impacts migraine. Concentration, energy levels, and mood can all be improved after a restful night of sleep—or impaired after a fitful night’s sleep. The consequences of sleep can often determine a productive day versus a reach-for-the-rescue-medication kind of day.
What Are Circadian Rhythms?
Sometimes referred to as the “body’s clock”, circadian rhythms refer to the physical, behavioral, and mental fluctuations that naturally occur over a 24-hour period. These clocks oversee various critical processes, one of which is the sleep-wake cycle. When this system becomes dysregulated, a multitude of health consequences can ensue.
Neurotransmitter Function
Neurons, or nerve cells, communicate with other cells via chemical messengers released in the brain. These neurotransmitters constantly work to keep the brain and body in proper function. From heart rate to mood, the neurotransmitter system is responsible for regulating critical biological processes.
During sleep, the neurotransmitter system receives a period of respite. This neurological hiatus is a notable benefit, as neurotransmitter dysregulation is implicated in migraine.10 Not only that but it’s also believed to be linked to depression and anxiety, conditions that are often comorbid with migraine.10
Cognition and Mood
From memory to mood, sleep impacts a range of cognitive processes. Impulse control, concentration, and memory consolidation can receive a boost after a good night’s sleep.2 In turn, learning and decision-making can be optimized, and productivity can be enhanced. The benefits of these perks mean better adherence to the healthy lifestyle habits that prevent migraine attacks and sleep problems.
On the other hand, poor sleep can negatively impact these outcomes, resulting in irritability, exhaustion, and mood swings. Consequently, following a migraine or sleep treatment plan can become difficult.
Weight and Glucose Control
Restorative sleep not only affects mental health but also aids in regulating glucose levels and weight. Given that migraine can be triggered by dips in blood sugar, achieving restful sleep can mitigate attacks induced by low blood sugar.2
Further, by keeping weight in check, sleep can combat obesity, which is believed to be a low-grade inflammatory state.11
Without these modulations in place, metabolic dysregulation can increase the risk of migraine progression.
The Glymphatic System: Detoxification
Interestingly, while you may be taking a break during a good night’s sleep, your brain is not.
“The brain is actually 10 times more active during sleep than it is while we’re awake, and some critically important tasks are going on while we’re sleeping.”1
One of these important processes is performed by the glymphatic system, otherwise known as the “garbage collector” of our brains. This detoxification process rids the brain of any toxins that were acquired during the day—a big plus for migraine, given that attacks can be triggered by environmental toxins.
However, in the absence of quality sleep, toxic waste can build up. Because the glymphatic system only functions during sleep, the cost of poor sleep can result in increased inflammation, another migraine trigger. Not only that, but the risk of dementia increases without this detoxification process.1
Pain Threshold
“Migraine patients who don’t sleep well are more vulnerable to terrible attacks than someone who is sleeping well.”1
Chronic sleep deprivation can lower the pain threshold and baseline level of functioning, something that is often already compromised in people with migraine.2 Without pain control, an individual may be primed for a tension headache or migraine attack upon awakening.
Conversely, a good night’s sleep can increase the pain threshold. By dampening down the pain response, quality sleep can decrease sensitivity to migraine triggers, effectively bolstering the capacity to weather migraine.
Summary
How Sleep Affects Migraine
Sleep drives a number of critical processes, and without quality sleep, physical and mental health may be compromised.
The neurotransmitter system, responsible for optimal cell-to-cell communication, gets reset after a good night’s sleep.
Memory, mood, decision-making, and concentration can either be enhanced or impaired by sleep.
Sleep regulates weight and glucose levels, thereby affecting metabolic function.
The glymphatic system rids the brain of toxins during sleep. Without this process, toxins may accumulate and contribute to inflammation.
The pain threshold can either be lowered by poor sleep or raised by good sleep.
Bottom Line
Migraine and sleep disorders share a bidirectional relationship driven by cycles of pain and poor sleep. Sleep apnea, insomnia, parasomnia, bruxism, and restless leg syndrome are common sleep disorders that are comorbid with migraine. A range of biological processes are affected by sleep, including neurotransmitter function, cognition and mood, weight and glucose control, detoxification, and pain processing.
FAQ Section
Additional Resources
- Why We Sleep By Matthew Walker
- Full Catastrophe Living by Jon Kabat-Zinn


