- Understanding Chronic Migraine
- Symptoms & Comorbidities of Chronic Migraine
- Why Some People Develop Chronic Migraine
- Diagnosis and Medical Evaluation
- The Role of Lifestyle in Chronic Migraine Management
- Medical Treatment Options for Chronic Migraine
- Non-Drug Approaches to Chronic Migraine Management
- Developing a Personalized Migraine Action Plan
- Conclusion
Chronic migraine is a neurological condition that can severely limit an individual’s quality of life. It can disrupt daily obligations, impacting mental health, and often lead to physical and social challenges.
To understand chronic migraine, it’s important to see how it affects people both physically and emotionally. Living with constant and unpredictable migraine attacks can create ongoing worry and stress, which can sometimes make the symptoms worse.
Through accurate diagnosis, appropriate treatment, and a few lifestyle adjustments, however, people with chronic migraine are often able to manage symptoms and improve their quality of life. This article will cover the essentials of chronic migraine: What it is, how it differs from other headache illnesses, and also what its symptoms, causes, risk factors, and treatment options are.
The goal is to help people with migraine better understand chronic migraine and offer strategies to manage symptoms, thereby reducing its impact on their lives.
Understanding Chronic Migraine
Chronic Migraine Defined
Before discussing the definition of chronic migraine, it helps to define what makes up a migraine attack.
As mentioned, migraine is a neurological condition that involves many symptoms, whereas the head pain often is the most prominent. Other common symptoms include nausea, vomiting, and sensitivity to light (photophobia) and sound (phonophobia).1
A migraine attack often includes moderate to severe headache pain that can last 4-72 hours, if left untreated.1 A typical migraine headache is described as throbbing pain on one side of the head that worsens with physical activity.1 Some people also experience an aura before the migraine, which may include temporary visual or sensory disturbances that gradually disappear.1
In addition to migraine with and without aura, there are additional types of migraine, which may include symptoms like dizziness, abdominal pain, weakness on one side of the body, and more. In this article you can find additional information about the different types of migraine. It is also useful to understand the different phases of migraine attacks.
Chronic migraine is defined by The International Classification of Headache Disorders (ICHD-3) when someone experiences headache on 15 or more days each month, for at least three months; and on at least eight of those days, the headache features typical migraine symptoms.2
This higher frequency of debilitating attacks in chronic migraine can lead to a near-constant state of pain and other migraine symptoms, often turning a person’s life upside down.
How Chronic Migraine Differs From Episodic Migraine
Chronic and episodic migraine are both types of migraine disorders, but they differ mainly in headache frequency and impact. According to The International Classification of Headache Disorders ICHD-3 beta criteria, episodic migraine refers to having less than 15 days a month with head pain and/or other migraine symptoms.3 Episodic migraine attacks occur less frequently and often allow more recovery time.
Pathophysiology of Chronic Migraine
Pathophysiology is the study of what goes wrong in the body to cause a disease or condition. It looks at how normal body processes get disrupted, leading to symptoms.
Although researchers still don’t fully understand what causes chronic migraine or why some people’s migraine attacks progress from episodic to chronic, it is believed that certain factors may play a role. This includes changes in how the brain processes pain, an increase in the brain’s sensitivity, and even structural changes in the brain itself.5
Researchers also believe it’s possible that people with chronic migraine are in a constant “warning phase” before an attack, which might keep these pain-processing changes active and make the brain even more sensitive over time.5 This is also known as central sensitization.
“The more frequently you get pain, the more frequently pain can cause itself. We have studies that show us that patients who have attacks that are frequent can start to have these processes in the brain where the brain is more sensitive, and it’s easier to get that next attack because the brain’s ready,” explains Dr. Jessica Ailani, a clinical professor of neurology at MedStar Georgetown University Hospital in Washington, D.C.
Prevalence & Global Impact of Chronic Migraine
About 14–15% of people worldwide are affected by migraine,6 making it a common condition on a global scale. Chronic migraine is estimated to affect 1-2% of the general population, and about 8% of people living with migraine.7
Did you know?
The 2019 Global Burden of Disease Study found that migraine is the second biggest cause of disability worldwide for both genders and all ages, and the first most common cause of disability among young women.8
Migraine contributes to approximately 4.9% of the global burden of ill health, measured in terms of years lived with disability (YLDs).6
More than one billion people worldwide live with migraine, with the highest prevalence among young adults.9 For most people living with migraine, the peak intensity occurs in their 20s and lasts until their 40s.9 This makes migraine a condition that significantly disrupts what should be some of the most productive years of life, during which individuals typically focus on education, career advancement, and starting families.
Migraine affects both men and women, but it is three times more common in women than men.10 For women, migraine occurrence is often related to changes in hormone levels. Attacks may start around the first menstrual period or arise during pregnancy when hormone levels shift significantly.10
These statistics highlight the significant role migraine plays in worldwide disability and the overall impact on health.
Symptoms & Comorbidities of Chronic Migraine
Common Symptoms of Chronic Migraine
People living with chronic migraine report a whole range of symptoms that often blend together along with the frequent headaches.11 While head pain can be disabling on its own, the additional symptoms can be even more disabling for people with chronic migraine. These include:
- Nausea and vomiting
- Loss of appetite
- Dizziness
- Constant sensitivity to light, sound, smells, or movement
- Neck pain
- Fatigue
Cognitive issues are also common among people with chronic migraine. Many individuals report feelings of brain fog, or just feeling like their brain is moving a little slower than normal. The following symptoms are examples of how this is often illustrated:
- Feeling confused
- Having trouble finding words
- Mood changes
- Trouble with concentration
Frequency, Duration & Severity of Attacks
When someone with migraine transitions from episodic to chronic migraine, the nature of their attacks often changes. Instead of having distinct attacks with a clear beginning and ending, people with chronic migraine may experience a continuous blur of head pain and other symptoms, making it difficult to pinpoint when one attack ends and the next begins.
Dr. Christine Lay, a professor of neurology at the University of Toronto and headache specialist who helps people living with chronic migraine every day, explains that this shift occurs because the brain’s pain threshold changes, making attacks easier to trigger even without clear causes.11
According to Dr. Lay, it is important for patients to take note in their migraine diary and talk to their healthcare provider about the days in between where they might not have a lot of head pain but may experience other symptoms.
Dr. Amaal Starling, a neurologist, headache specialist, and associate professor of neurology at the Mayo Clinic College of Medicine, agrees with Dr. Lay, and says that people living with chronic migraine often do not give the whole picture when they talk to their healthcare provider.
Dr. Starling says she asks her patients these two questions to help determine a more accurate diagnosis of chronic migraine:12
- How many days per week or per month are you having headache or any migraine symptoms?
- How many days per week or per month do you have zero headache or migraine symptoms whatsoever?
Comorbidities to Chronic Migraine
Comorbidities are other health conditions that often occur alongside a primary condition. People living with migraine have a range of comorbidities, the most common being:13
- cardiovascular disease (including stroke and heart attack)
- depression and anxiety
- sleep disorders (including insomnia and restless legs syndrome)
- other pain disorders (like fibromyalgia and back pain)
Studies show that these comorbidities are more common in people with chronic migraine than in people with episodic migraine.13
In addition, Dr. Dawn C. Buse, psychologist and clinical professor at Albert Einstein College of Medicine, adds the following comorbidities to being common for people living with migraine:28
- epilepsy
- multiple sclerosis (MS)
- panic disorders
- suicidality
- nonsuicidal self-injurious behavior
Hoping to squash the stigma, Dr. Buse stresses that people with comorbidities shouldn’t feel bad, guilty or embarrassed because life with migraine is life with comorbidities. She says that if someone doesn’t have any comorbidities, then they are the most rare unicorn, because almost everyone’s going to have them. It has to do with all sorts of genetic predispositions, neurotransmitters, inflammation, things happening systemically in the whole body, as well as external forces, both environmental and social.
It is important to share all your symptoms with the healthcare professional caring for your migraine. Other medical conditions may affect your headache diagnosis. Also, some headache treatments are unsafe or contraindicated in people with certain conditions or who are on certain medications that may have negative interactions.13
Dr. Buse says there is some data that shows that if one of these conditions gets better, the others might as well. They kind of travel together. She advises that it’s a good thing to actively treat as many of your comorbidities as possible — or at least monitor them for safety.
Dr. Rebecca Burch has studied migraine comorbidities as part of her research through Brigham and Women’s Hospital at Harvard Medical School. In this video she explains more about mood disorders that are highly comorbid with migraine. Which comes first, the pain or the depression? The video is from the 2021 Migraine World Summit.
Read more about migraine and mental illness.
Impact on Daily Life & Mental Health
Living with chronic migraine involves much more than just coping with intense and frequent head pain. This condition can significantly reduce the quality of life for those affected, and can often impact a person’s self-esteem and confidence, as people may feel misunderstood or judged by others who don’t fully understand their condition.
Chronic migraine often results in social isolation, as people avoid potential triggers or fear having another attack when away from home. This can lead individuals with migraine to limit their enjoyment of daily activities and engagement with loved ones, hobbies, work, and other meaningful life events, leaving them feeling isolated and disconnected from the world.
The frequency of attacks and time spent in pain and other debilitating symptoms often leads to physical limitations, making exercise and movement challenging. Chronic pain can also disrupt sleep, and together these effects can create a negative cycle and affect one’s overall well-being.
Chronic migraine can also lead to feelings of anxiety, depression, irritability, and emotional exhaustion due to the unpredictable nature of attacks. Cognitive difficulties like brain fog and difficulty concentrating or remembering can be common both during and in between migraine attacks for those living with chronic migraine. This can be especially difficult to deal with in a work setting.
Chronic migraine can also lead to financial stress due to missed workdays, decreased job performance, and healthcare costs for treatment and medications.
Chronic Migraine & Mental Health: When It’s Time To Do Something
The disappointment of failed treatments, guilt from missed commitments, the strain from suffering relationships, and the fear of the next attack are common feelings for someone living with chronic migraine. It’s a burden that is carried on top of a chronic disease that can leave someone feeling isolated and unfairly judged.14
How does one know when their mental health has become a problem that needs to be addressed? This is how Dr. Buse views this question:
… When you feel you’re not living life as you’d like, you might notice it affecting work, school, or a loss of interest in hobbies or social activities. This isn’t just the burden of migraine making things hard to do; it’s feeling like you don’t want to anymore. That’s likely a sign of depression, and it’s worth discussing with a healthcare professional, like your primary care doctor.
Why Some People Develop Chronic Migraine
Common Causes & Risk Factors
Migraine attacks are believed to happen due to a mix of brain sensitivity, genetic factors (most people with migraine have a family history of it), and the body’s reaction to stress or hormonal changes.15 This leaves women particularly vulnerable due to hormonal fluctuations throughout their lives, including puberty, menstruation, pregnancy, and menopause.
Over time, some people with episodic migraine experience an increase in attack frequency, leading to chronic migraine. This transformation can be driven by underlying neurological changes, such as central sensitization, a process where the brain and nervous system become more sensitive to pain signals. For a person living with migraine, this can feel like anything and everything triggers an attack.
This process can be seen as a threshold issue: a combination of predisposing factors and repeated headache episodes gradually lowers the brain’s tolerance for migraine attacks, making the transition to chronic migraine more likely.7
Although the reasons why episodic migraine can turn into chronic migraine are complex, some factors that increase the risk of this progression include:
- Obesity 7
- Depression7
- Asthma12
- Sleeping disorders12
- Other pain disorders12
- Lower educational status7
- Stressful life events7
- Acute medication overuse7
- Ineffective acute treatment7
Dr. Lay explains how this last bullet point can do a lot of damage.
… You often end up doing more harm than good if you’re a patient who says, ‘I don’t want to take any preventive; I’ll just tough it out. And I’ll wait and take my triptan when I’m [having] a red headache, and I’m in bed and sick.’ You’re actually just increasing the burden, and you’re increasing your disability, and we don’t think it’s good for your brain.
Dr. Lay also discusses grappling with taking acute medication early enough while, at the same time, trying to avoid medication overuse headache, further explained below. This video is from the 2022 Migraine World Summit.
Diagnosis and Medical Evaluation
Definition and Diagnostic Criteria (ICHD-3) for Chronic Migraine
The International Headache Society has published a comprehensive classification system that organizes all types of headache disorders in a detailed, hierarchical format. This system serves as a resource for accurate diagnosis and standardized research across headache-related conditions.
To get the diagnosis “chronic migraine” a person needs to fulfill these criteria set by the International Classification of Headache Disorders (ICHD-3):2
A: You have headaches that feel like migraine or tension-type headache on at least 15 days per month for over 3 months, and fulfill criteria B and C.
B: You have had at least five previous attacks, meeting the standard criteria for migraine (either with or without aura), and fulfilling criteria B-D for 1.1 Migraine without aura and/or criteria B and C for 1.2 Migraine with aura.
C: On at least 8 days each month, for more than 3 months, you have headache that meets any of the following:
- criteria C and D for 1.1 Migraine without aura
- criteria B and C for 1.2 Migraine with aura
- Feels like migraine when the attacks start and is relieved by medications like triptans or ergot derivatives.
D: Not better accounted for by another ICHD-3 diagnosis.
Conditions That Can Present Like Chronic Migraine
Certain conditions share symptoms with chronic migraine, making accurate diagnosis challenging. Status migraine, also called status migrainosus, is a debilitating migraine attack that lasts for more than 72 hours.16
Another similar condition is medication overuse headache (MOH). This is also often called rebound headache, and typically occurs when someone takes acute pain medications more frequently than recommended over a period of three months or longer.17
Studies from various countries show that more than half of individuals experiencing headaches 15 or more days per month have MOH.18 Clinical observations reveal that most patients with MOH see an improvement in their symptoms after stopping the overuse of medication, which also enhances their response to preventive treatments.18
High-frequency episodic migraine (HFEM) refers to experiencing 8-14 migraine attacks per month. While this term is not yet an official classification in the International Headache Society’s system, it is gaining recognition in headache research and clinical practice.27
New daily persistent headache (NDPH) is a type of chronic daily headache that can be similar to chronic migraine. This headache does not build up over time, but starts suddenly and becomes a chronic daily headache right from start.4 People usually remember the exact day it started. The pain can feel like a migraine attack, a tension-type headache, or even a mix of both, but it does not have any defining features that make it easy to classify as one or the other.4
Importance of Accurate Diagnosis
Since chronic migraine can often resemble other headache disorders, a thorough evaluation by a healthcare provider is critical. Getting an accurate diagnosis is key to managing chronic migraine and improving a person’s quality of life. It helps a healthcare provider understand which treatment options are best suited for their patient.
Without a precise diagnosis, patients may receive treatments that don’t address the underlying issues, potentially leading to unnecessary side effects or even worsening their symptoms.
Role of Neurologist/Headache Specialist
Primary care physicians are often the first to diagnose and treat people living with migraine. They may prescribe migraine medications, recommend lifestyle changes, and refer patients to specialists if needed.
While finding a headache specialist can be challenging due to their limited availability, neurologists are often a helpful alternative since they frequently treat migraine patients. Not all neurologists specialize in headache, but many are experienced in diagnosing and managing migraine disorder, making them a valuable resource for those struggling to find effective relief.
The Role of Lifestyle in Chronic Migraine Management
Lifestyle changes are proven to help reduce migraine.12 The SEEDS approach, recommended by experts like Dr. Starling,22 focuses on:
Exercising regularly
Eating a healthy diet
Drinking water
Stress management

Consistent sleep routines, regular exercise (starting small if necessary), balanced meals, and staying hydrated can all help reduce migraine frequency and severity.
There’s no universal migraine diet because triggers vary between individuals. It is helpful, however, for people living with migraine to recognize personal patterns when it comes to food and beverage, rather than follow a strict diet.21
When it comes to stress management, the goal isn’t necessarily to eliminate stress entirely, but techniques like mindfulness, biofeedback, and relaxation can empower individuals to cope more effectively.22
Medical Treatment Options for Chronic Migraine
Preventive Medications for Migraine
Preventive medication for migraine comes in various options, but all have the same purpose: To reduce how often a person gets migraine attacks and reduce the impact that migraine has on their life, or ideally, both.
First-line treatment options for migraine prevention include:
- Anti-seizure medication
- Blood pressure-lowering medication, including beta blockers and calcium channel blockers
Other approved treatments for migraine prevention include:17
- Antidepressants
- Gepants
- Calcitonin Gene Related Peptides (CGRP) monoclonal antibodies (mAbs)
- OnabotulinumtoxinA (Botox)
For people living with chronic migraine it might take time to find the right preventive medication. Many also experience that they need to use more than one preventive medication to get an adequate effect. A combination of preventive medications may have a positive synergistic effect.23
Learn more about preventive medication for migraine.
Did you know?
The American Headache Society (AHS) has released an updated consensus statement advocating for the use of calcitonin gene-related peptide (CGRP)-targeting therapies in migraine prevention. They encourage that these treatments should be considered first-line options alongside with today’s approved first-line preventive medications, without the necessity of trying and failing other treatment classes first.29
Finding the Right Treatment for Chronic Migraine
When someone is living with chronic migraine, it is essential to have a treatment plan that addresses both immediate migraine relief and long-term prevention. Different types of over-the-counter and prescription medications, both acute and preventive, can complement each other effectively. Lifestyle alterations can also have a significant impact.
According to Dr. Lay, there are definitely alterations in the structure of the brain due to chronic migraine. It’s not fully understood why this happens or what’s going on in the body and brain to cause it, but she says they do know it is possible to change it.
We don’t really fully understand how or why, but we do know that doing all the right things, such as lifestyle factors, [nutritional supplements], getting out for a walk, mindfulness, meditation, treating your attacks when they come, getting on top of them early, and looking at preventive therapy, are all really important to reverse from chronic migraine to episodic migraine, but also to reverse some of those brain changes.
Non-Drug Approaches to Chronic Migraine Management
In addition to migraine medication, newer treatments suggest that alternative approaches, like complementary and integrative therapies, can aid in migraine attack prophylaxis and help reduce the disability that often comes with chronic migraine.25 This can make a big difference for people dealing with the daily impact of migraine.
These options range from biobehavioral therapy, which includes techniques like biofeedback, mindfulness, and cognitive behavioral therapy (CBT), to acupuncture, shown to help reduce migraine frequency when done consistently.25 Studies are showing about 8-10 sessions are needed to determine if acupuncture is helpful in reducing migraine frequency. And these are usually twice a week.25
Learn more about biobehavioral therapy.
Physical therapy can address contributing factors like neck tension or TMJ,25 while neuromodulation devices target nerve activity to alleviate or prevent attacks.
Read more about the different types of neuromodulation devices.
Emerging treatments like brain retraining focus on rewiring brain pathways to manage chronic pain. Dr. Bethany Ranes, a cognitive neuroscientist, whose field bridges neuroscience and psychology, explains what happens by doing brain retraining.
“Brain retraining works by focusing on the pathways, or connections, in our brain that control our bodies. These pathways are like roads that brain cells use to communicate and interact.“We used to think these pathways were fixed, especially after childhood. But new technology has shown us that we can change them, even as adults.”
Learn more about resilience training.
Dr. Ranes talks about the “Boulder Back Pain” study that is used as evidence that brain retraining, specifically pain reprocessing therapy, is an effective strategy for treating chronic pain. The video is from the 2022 Migraine World Summit.
Developing a Personalized Migraine Action Plan
Coping with Migraine Stigma
A common stigma surrounding migraine is that it’s “just a bad headache” that’s easy to fix. Many people with migraine fear being seen as weak and lazy, or that it’s “all in their head,” or even that they’re faking it.
Dr. Robert Shapiro, a professor of neurological sciences at the University of Vermont, explains one excellent way to combat the stigma.
“The method that has been reported to have the most effectiveness is what’s called ‘contact.’ Contact is, quite simply, someone who carries a stigmatizing attitude interacting directly with somebody who is stigmatized.”
He reiterates, “So educating yourself about the disease is really a helpful thing, so that you can explain to others what you’re experiencing.”
Learn more on migraine stigma.
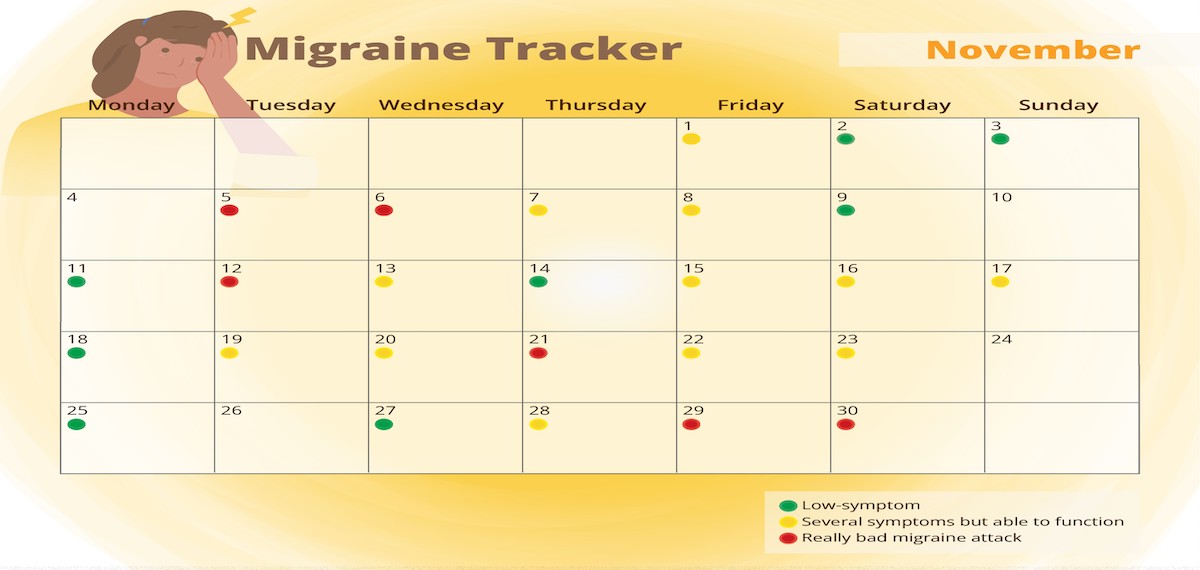
Tracking Headache Patterns & Triggers
For people living with migraine it can be useful to keep a migraine diary to keep track of migraine attacks and symptoms, medications used, and medication effects.
Many people with migraine have a tendency to only keep track of the very bad days, but it is also very important to keep track of days with milder head pain, as well as days affected by other symptoms.
Dr. Lay explains, “There are a number of different symptoms that go along with that head pain: feeling confused, having trouble finding words, the light, sound, and smells that are bothering you, your clothing bothering you, feeling like you’ve lost your appetite, frank nausea, even vomiting. So, what I encourage my patients to do is to keep track of the headache because that’s sort of the first clinical sign that a migraine is underway for many of us. So, you must write down those headache days. But I do have patients track other days, as well. And I want them to make note of crystal-clear days and, a truly migraine-free day, not just a headache-free day, but a migraine-free day.”
Collaborating with Healthcare Providers
Working closely with healthcare providers is essential for the effective treatment of chronic migraine. By openly sharing one’s symptoms, triggers, and any changes in their condition, a patient can help their provider understand their unique needs and tailor a treatment plan accordingly.
Regular check-ins allow for adjustments to medication, lifestyle recommendations, and preventive strategies. Building a strong partnership with one’s healthcare team can lead to better outcomes, as the practitioner can support the patient in finding the most effective ways to manage and reduce migraine attacks over time.
Creating an Emergency Kit for Migraine Attacks
When managing chronic migraine, a person may have more migraine days than the number of days they are recommended to use acute medications. For this reason, it can be helpful to have an “emergency kit” with alternative options to offer support on migraine days.
What to put in the kit is up to the individual. It depends on what their biggest migraine triggers or symptoms tend to be. Maybe a person is really sensitive to light and sound, or maybe it’s nausea that is the most disabling. Others find that a hot or cold compress can help provide distraction from pain and reduce inflammation. Avoiding dehydration is also important. That said, here are a few examples of what to include in the kit:
- Acute medication — medication that helps stop an attack once it’s started
- Sunglasses, migraine glasses, or an eye mask — to help with light sensitivity
- Earplugs or noise-canceling headphones — to help with sound sensitivity
- Cold or warm compresses — to help relieve inflammation and distract from the pain
- A water bottle and electrolytes powder — to assist in staying hydrated
- A migraine cooling/menthol stick/roll-on — to help soothe attacks with a cooling sensation
- A neuromodulation device — modulates nerve activity to block pain signals, helping to prevent or stop attacks
- A Reliefband — relieves nausea through emitting pulses that stimulate the median nerve, normalizing the nerve messaging from the brain to the stomach

Self Care Strategies
Coping mechanisms and self care are vital tools for managing the challenges of chronic migraine. By practicing self kindness rather than self stigmatizing, or blaming oneself for an attack by thinking, “I stayed out too late” or “I didn’t take care of myself,” is essential to hold onto.
Acceptance also plays a big role for people living with migraine. Acknowledging that migraine is a neurological, biological disorder, and that it is not the person’s fault that they get migraine attacks, may allow the person to shift their energy toward proactive management, rather than self blame, and work to improve their quality of life.
Practicing self care also means listening to one’s body’s needs, such as resting during a migraine episode. Identifying and setting boundaries, both in personal and professional settings, can help prevent overexertion, which may worsen symptoms.
Support Systems
Seeking emotional support through friends, family, or support groups can provide a sense of community and reduce feelings of isolation. A good support system can affect a person’s quality of life a great deal.
Dr. Lay’s advice is for people with migraine to open up to a few people who they trust, and educate them about what migraine is, and how it is to live with migraine.
“It really is a battle day-by-day, but that’s why it’s really important to engage with your provider, number one, but also, let a few people in,” says Dr. Lay. “Let them know what’s going on, let them understand how burdensome this migraine is. It’s not simply a headache.”
Conclusion
Key Takeaways for Patients & Caregivers
- Chronic migraine is a complex neurological condition that can deeply impact daily life, mental health, and physical well-being.
- Patients and caregivers should understand both the physical and emotional aspects of living with migraine, as well as the importance of a comprehensive treatment plan.
- While each person’s experience is unique, early diagnosis, personalized treatment, and lifestyle adjustments can greatly improve quality of life.
- By building a strong support system and keeping track of symptoms and triggers, patients and caregivers can work together to better manage the condition.
- For those living with migraine and their caregivers knowledge is power. Understanding the essentials of migraine management can make a meaningful difference in daily life.
The Importance of Early Diagnosis & Comprehensive Care
Detecting migraine early and receiving thorough care can greatly improve outcomes for those affected. An early diagnosis helps individuals understand their condition sooner, allowing them to manage symptoms before they worsen or become chronic.
Working closely with healthcare providers ensures that each aspect of migraine management is considered, leading to a better quality of life and potentially reducing the frequency and intensity of attacks.
The Outlook for People With Chronic Migraine
One thing that is important for people living with migraine to know, is that chronic migraine is reversible. Around 26% of people who develop chronic migraine go into remission within two years of their condition becoming chronic.7
“The one thing we really don’t want people who are suffering from chronic migraine to do, is to lose hope. Because there’s always hope. It’s a really exciting time in terms of science. We’re understanding more, we’re making newer, different, targeted medications. We also understand more about the importance of things like mindfulness and meditation, and understand now that meditation is critically important,” Dr. Lay says.
There is even hope for those who have felt stuck in chronic migraine for years.
Dr. Lay adds, “We do think that the longer you’re stuck in chronic migraine, the harder it is to get out of it. We know that certain things are good for you to do when you have migraine, but when you have chronic migraine and you’ve got a disabling attack 20, 25, 30 days a month, it’s really hard to follow those lifestyle changes. So, I do think the longer you’re in it, the harder it is to break the cycle, but it doesn’t mean we can’t break the cycle.”