Those who persevere through migraine know all too well the struggle that comes with living with this debilitating disease. The nausea, agonizing head pain, sensation disturbances, temporary cognitive impairment, and the general feeling of lost control over their own bodies. While there are many types of migraines, those living with vestibular migraine live a unique struggle when it comes to managing their attacks.
What is Vestibular Migraine
Migraine is considered a complex neurological condition. Vestibular migraine is unique within this class. Vestibular migraine is often referred to by its nicknames, “dizzy migraines” or “migraine-associated dizziness,” also “migraine-associated vertigo,” and “brain stem aura” by patients who suffer from pronounced vestibular symptoms associated with their migraine.1
Definition
The term “vestibular” refers to the sense of balance, spatial orientation, and more specifically, the structure of the inner ear.
Symptoms of Vestibular Migraine
Similar to classic migraine, vestibular migraines have a multitude of debilitating symptoms. Recent literature has classified these symptoms into two classes: ictal and interictal. This classification system is synonymous with the categorization of chronic migraine symptoms as primary and secondary. Ictal symptoms tend to occur during a migraine attack, while interictal symptoms trigger during remission of an attack.2
The most common symptom associated with vestibular migraine is vertigo or dizziness. Most patients also report dizzy sensations, such as constant falling, rocking back and forth, out-of-body experiences, and spatial disorientation. “Alice in Wonderland Syndrome” is a clinical term that refers to a severe perception of viewing the world from a shrunken standpoint due to spatial disorientation.3
It is important to distinguish that vertigo can occur with or without a headache. It is also crucial to understand that vertigo can coincide with common migraine symptoms such as:
- nausea
- constipation
- mood changes
- polyuria (increased urination)
- confusion
- sensitivity to sounds and smells
- visual aura
- lightheadedness4
- problems with hearing
- problems with taste and/or smell
- body aches (i.e., shoulder pain, and neck and back pain)
The rate of the brain’s recovery, from vestibular migraine, is the same as a classic migraine patient: it takes time for the brain to recover from any migraine attack and the time period of recovery is variable for every person.2
What Causes Vestibular Migraine
If getting a proper diagnosis is enervating enough, pinpointing the triggers and the exact origin of vestibular migraine is just as perplexing, even to the experts in the field of migraine research. Over the years, many competing theories have emerged to try to explain the pathophysiology of this devitalizing condition. The triggers, however, have gathered more of a consensus among the experts.
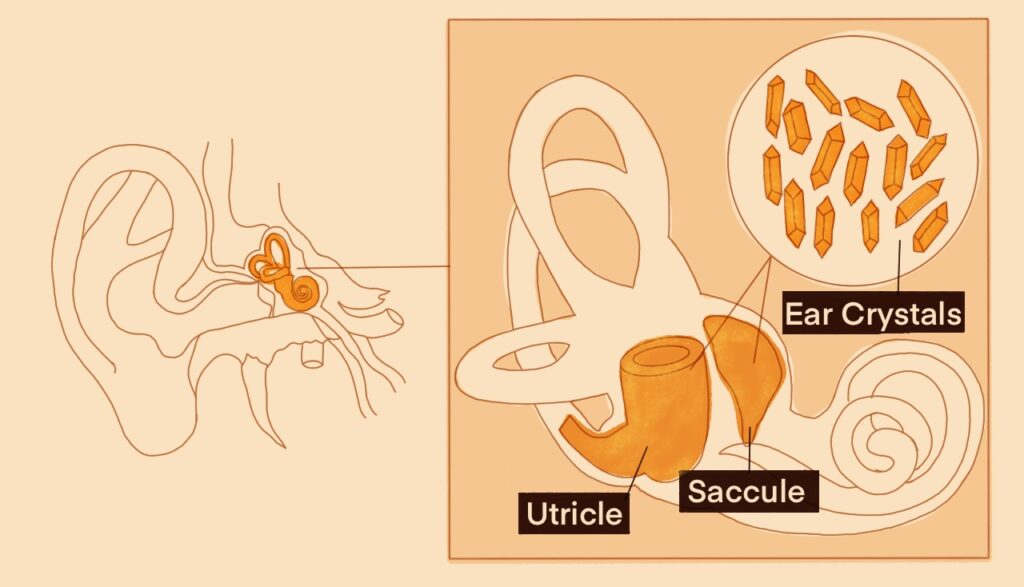
Vestibular migraine has similar triggers to those of typical/classic migraine, such as:
- changes in weather patterns
- stress
- menstruation/menstrual cycle changes
- skipping meals
- intolerance to certain foods/food triggers
- dehydration
- lack of sleep
The truly unique triggers of vestibular migraine are:
- exposure to a lot of head movement
- overload of visual stimuli2
Over the years, there have been many competing theories that have emerged to try to explain the pathophysiology of this devitalizing condition. The three leading theories that surround the common cause of this type of migraine are:
- structural problems found in the inner ear
- coexistence with Meniere’s disease and BPPV (Benign Paroxysmal Positional Vertigo)
- dysfunction of the vestibular pathway
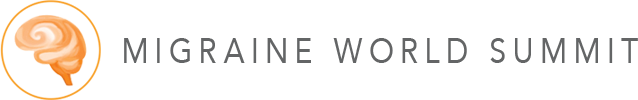
Structural inner ear problems
In the structure of the inner ear, there are microscopic crystals that help us maintain our balance. Just the same as our bodies constantly replenish us with new blood cells and skin cells daily, crystals found within the inner ear eventually fall off, get dissolved, and are soon replaced with new ones. However, as we age, the rate at which we lose these crystals becomes higher and occurs much more often, which leads to an accumulation of loose crystals rattling in the ear canal, which is regarded to be the cause of vertigo.
In patients with vestibular migraine, the process of losing crystals at an accelerated rate seems to occur in young patients rather than normal crystal loss seen in older patients. The shedding of these crystals seems to cause injury to the part of the inner ear called the otolith organ. Once these crystals become loose, they can trigger bouts of vertigo, as seen in patients with a similar condition known as BPPV. The clinical implications suggest that the displacement of these crystals could lead to mild hearing loss at later stages of life.2
Coexistence with Meniere’s disease and BPPV
Meniere’s disease, BPPV, and vestibular migraine are similar in many ways, but the statistics that surround them are not to be mistaken as a coincidence. Experts have found the following statistics:
Meniere’s disease statistics
56% of Meniere’s patients, within the general population, have migraine
85% of patients with Meniere’s disease, found in both ears, have migraine
This theory suggests that there could be a possible spectrum in which patients could fall between these two conditions. Some patients may suffer specifically from inner ear issues, while other patients, with migraine, suffer a fall during an attack, which then could turn into Meniere’s disease.5
The statistics surrounding BPPV in migraine patients also suggest a clinical trial relationship. Around 22% of patients with vestibular migraine are found to have loose crystals. In one clinical trial, of 500 vestibular migraine patients, 47% were found to have BPPV. However, experts also found 22% of that group actually had been diagnosed with BPPV at the same time of their vestibular migraine initial diagnosis.5
Dysfunction of the vestibular pathway
Similar to classic ordinary migraine, disruptions in the neural pathways are commonly cited as a cause for vestibular migraine is a common explanation. The consensus, among this theory, suggests that the disruptions seen in the vestibular pathway are not solely caused by injury, but rather by poor functionality.4 This theory also suggests that, similar to how there are changes seen in the visual processing center of the brain in classic migraine patients, which produce a visual aura, the changes seen in the vestibular processing may be triggered by change because of activity in the vestibular nuclei. Other interconnected pathways seem to be affected (vestibular nuclei, other structures, and blood vessels).5
Diagnosis of Vestibular Migraine
Vestibular migraine is often misdiagnosed due to its symptoms masquerading as other vestibular disorders.
Vestibular migraine often misdiagnosed as
BPPV (Benign Paroxysmal Positional Vertigo)
PPPD (Persistent Postural-Perceptual Dizziness)
Meniere’s disease
sinusitis
tinnitus
concussion
BPPV (Benign Paroxysmal Positional Vertigo)
BPPV is a condition characterized by brief sessions of mild to severe dizziness, often triggered by changes in head position.6 This condition’s origin is set among the crystals in the structure of the inner ear that become loose and get lodged in canals of the ear that maintains balance. The difference between BPPV and PPPD is the length of vertigo spells. A patient with BPPV typically experiences about 30-40 seconds worth of episodic vertigo while PPPD patients’ vertigo seems unrelenting.
PPPD (Persistent Postural-Perceptual Dizziness)
PPPD is a condition that is closely related to BPPV. The main difference between the two is that with PPPD, the patient has persistent dizziness, unsteadiness, and disequilibrium that can be triggered by any condition that causes vertigo. The condition is also associated with vestibular migraine because of the repeated attacks of vertigo.2
Meniere’s disease
Meniere’s disease affects the inner ear and can cause the patient to experience episodes of dizziness and hearing loss. The cause is unknown but is believed to be attributed to fluid imbalance or accumulation in the inner ear. Its symptoms overlap with sinusitis with patients reporting fullness or pressure in the ear and changes in hearing levels, and tinnitus (ringing in the ear.) Similar to migraine patients, those with Meniere’s disease also report phonophobia (aversion to loud noises) and photophobia (aversion to bright lights).
Vestibular migraine differs from Meniere’s, PPPD, and BPPV as the dizziness associated with this disease tends to occur along with the neurological symptoms that are typically seen with migraine.
Sinusitis
Sinusitis is the inflammation of the membranes found within the sinus cavity. Because 90% of patients report facial pressure, this could lead to the improper diagnosis of sinusitis or sinus headache rather than what could most likely be vestibular migraine.7
Tinnitus
Tinnitus is defined as a condition where a patient hears a constant ringing sound without the presence of an accompanying external sound. The prevalence of vestibular migraine in conjunction with tinnitus is high enough that most clinicians would consider there to be possible links between them.2 About half of people who are diagnosed with vestibular migraine also report tinnitus symptoms while another study found 80% of patients reported a spinning sensation.
Concussion
At the extreme end of the diagnostic spectrum, vestibular migraine could be misdiagnosed as a concussion. Of course, the likelihood of this diagnostic mistake is considerably low without the instance of a head injury. People who suffer a concussion can have dizziness or vestibular symptoms of ringing or other sounds within the ears.8
Given the overlapping symptoms in many vestibular conditions and vestibular migraine, getting a proper diagnosis can be challenging. To make matters worse, many patients experience another hurdle in getting an accurate diagnosis: how to find the right specialist?
Neurologists and Ear, Nose, and Throat specialists (ENTs) are the most common specialists who receive patients who report vertigo and dizziness. However, one of the main issues with this referral paradigm, while it seems innocent, is that ENTs are not adept at managing vestibular migraine patients’ treatment plans in an ever-changing treatment landscape. And the other is that while neurologists are familiar with how to navigate the medication landscape, vestibular migraine is still a relatively poorly misunderstood condition, even among the experts in this field of specialists.2
The best answer for which specialist a patient fitting the criterion for vestibular migraine should seek out is one who has training in ear medicine and ear neurology. This specialist may go by the following names, depending on the department in which they work:
- otoneurologist: A neurologist who also specializes in ear conditions
- neurotologist: A specialist who specializes in both otology and neurological conditions pertaining to the ear.5
Unfortunately, there is no specific test for diagnosing vestibular migraine. Researchers currently classify it as following a “classic migraine pattern of disease.” Meaning a patient goes to their doctor reporting an increase in headaches and other neurological symptoms, including dizziness.5
Recently, as of 2019, the International Headache Society constructed the term “vestibular migraine” in order to ensure stricter diagnosing criteria and to continue the study of vestibular migraine in greater depth. Unfortunately, while criteria like this are useful in biological and clinical efficacy trials, it presents a problem when people use the criteria as means to learn about the disease further. However, vestibular migraine is still a relatively new condition. So much so, in fact, it is surprising that most medical schools don’t teach vestibular disorders in their curriculum.2 As a result, the hallmark symptoms of vestibular migraine, i.e., dizziness and vertigo, are unfortunately not widely hot topics in the medical community. Thus, the diagnostic criteria are still relatively new as the condition is still coined as “new” based on its low understanding by experts.2
The next question would then be if getting an accurate vestibular migraine diagnosis is not any easier than managing symptoms, are there consequences of not getting a proper diagnosis early? Well, the answer is simple: the consequences would follow a similar trajectory as any other chronic condition that is ignored. The patient is likely to experience worsening symptoms relating to their vestibular migraine, particularly their interictal symptoms.
Who Gets Vestibular Migraine?
Previous studies’ statistics have observed the following conclusions:
- Young women in particular, who have recurrent vertigo, migraine is the most likely diagnosis.4
- Vestibular migraine tends to occur in people who are in their late 30s and older.2
- Vestibular migraine tends to affect people following menopause. While patients tend to suffer from migraine headache attacks during their reproductive years, the headaches tend to improve once menopause occurs, then manifestations of vertigo and dizziness tend to set in soon after menopause.
- The prevalence rate of vestibular migraine in children is between 0.7%- 15%.9
Migraine disease is tricky to pinpoint susceptibility. But common consensus agrees that the diagnosis of migraine largely has to do with certain pathophysiologic mechanisms. If we are to approach this from the nature versus nurture epidemiological debate, science has determined that the genetic and environmental factors are split either 50-50 or 60-40. However, the genetic expression of migraine can vary even within an individual’s family, where it is possible this expression can be very different.5 It bears noting that patients with migraine have a low threshold for certain stimuli. In the case of vestibular migraine patients, the sensitivity of balance and tilting tends to be greater compared to individuals without migraine.5
Treatments for Vestibular Migraine
Luckily for those who are afflicted with vestibular migraine, there is a wide range of treatments available to ease symptoms and improve quality of life.
Healthcare providers advise patients to establish an ACTION plan to manage and treat their migraines. The ACTION plan is broken down into five categories.
ACTION plan
A (alternative therapies)
C (changes)
T (therapeutic options)
I (interictal symptom management)
O-N (planning to move “on”)
Step “A” (alternative therapies)
The first part of developing an ACTION plan is to consider alternative therapies (Step “A”). Alternative therapies include vitamins, herbs, nutraceuticals (a substance that is a food or a part of a food that has medical or health benefits), and exercises that are fitted to the individual.
Step “C” (changes)
Part two of the ACTION plan is to implement changes (Step “C”). This stage of the sequence involves two parts. It is necessary to identify triggers and avoid them in this step. The changes that take place can be little or big changes. Examples of this would be creating a diet that you can stick to or one that is specifically tailored to be anti-inflammatory, reducing the number of stress triggers, and avoiding food triggers.
Step “T” (therapeutic options)
Part three is to explore therapeutic options (Step “T”). This involves finding preventive and acute medications that fit your symptoms and lifestyle. This is the step with the most trial and error. This could be the most frustrating part of the sequence that can span years. Even if a medication is effective, it can become less effective over time, which could lead to searching for a new option.
Step “I” (interictal symptom management)
Part four is specifically catered to treating/managing interictal symptoms (Step “I”). This is the step that requires a dispelling of stereotypes around migraine. The ongoing challenge in managing migraines is a reminder that symptoms are truly more than the sum of their parts. It’s never “just a headache” or “dizzy spells.” Migraine attacks are much more complex than many realize. Learning to manage migraine symptoms is also the key to preventing other comorbidities (the presence of two or more diseases or medical conditions) that are more likely to occur with a migraine diagnosis, such as anxiety, depression, insomnia, sleep apnea, and motion sensitivity, also known as motion sickness.
Steps “O-N” (planning to move on)
The final part of the ACTION plan is a simple reminder to have faith that things will get better (Steps “O” and “N”). Now granted, that’s easier said than done. While it can seem migraine takes center stage in most people’s lives, it can be managed in a way that it takes occasional precedence. This part of the plan also encourages the need to make steps toward planning a life with migraine, rather than planning life around it. While migraine is chronic, establishing an optimistic future for yourself (e.g., manageable goals, lifestyle changes, future aspirations) and a solid support system are the golden tickets to living positively with migraine.2
Drug Therapies
Experts agree that when exploring drugs to combat vestibular migraine, the treatment of vestibular migraine is not that different from treating chronic migraine. Similar to chronic migraine, vestibular migraine needs to be treated with preventive medication. The medications to treat chronic migraine are divided into four classes, but vestibular migraine includes a few categories of its own.
The typical course of treatment for vestibular migraine follows the same trajectory as classic migraine utilizing various drug modalities. Current treatment option categories include:
- triptans
- sodium versus calcium channel blockers
- beta blockers
- antidepressants
- CGRP inhibitors
- selective serotonin reuptake inhibitors (SSRIs)
Classification of drug treatments for vestibular migraine
| Treatment | How it works | Type of treatment | Common side effects | Commonly prescribed examples |
|---|---|---|---|---|
| Triptans11 | Serotonin Receptor Agonists; shrinks swollen blood vessels in the brain | Acute | Dizziness, weakness, nausea, sleepiness, pain at the injection site, pain in nasal passages | sumatriptan (Imitrex), sumatriptan/naproxen sodium (Treximet), zolmitriptan (Zomig), eletriptan (Relpax) |
| Sodium channel blockers12 | Anti-seizure medication; slows or blocks the sodium channel | Preventive | Dizziness, nausea, vomiting, problems with coordination, balance, and speech, double or blurred vision, rash, itching, headaches, changes in blood pressure, weight gain or loss, fatigue, sleepiness, insomnia, hair loss, tremors | topiramate (Qudexy XR, Topamax), valproic acid (Depakene, Depakote) |
| Calcium channel blockers13 | Blood pressure medication; eases the narrowing of blood vessels | Preventive | Fatigue, heartburn, facial flushing, swelling in the abdomen, ankles, or feet | diltiazem (Cardizem, Cartia, Tiazac), verapamil (Calan, Covera HS, Verelan) |
| Beta blockers14 | Blood pressure medication; relaxes blood vessels and slows heart rate | Preventive | Slow heart rate (bradycardia), low blood pressure (hypotension), irregular heart rhythms (arrhythmias), fatigue, dizziness, nausea, insomnia, sleep changes, nightmares, dry mouth or eyes | metoprolol (Lopressor, Toprol XL), nadolol (Corgard), propranolol (Inderal, Inderal LA, Inderal XL, InnoPran) |
| Tricyclic antidepressants16 | Increases amounts of serotonin and norepinephrine | Preventive or acute | Dry mouth, nausea, nervousness, restlessness, insomnia, blurred vision, constipation, drops in blood pressure when standing, urinary retention, drowsiness | amitriptyline (Elavil), nortriptyline (Aventyl, Pamelor) |
| CGRP inhibitors15 | Blocks the molecule involved in causing migraine pain | Preventive or acute | Hypersensitivity allergic reactions, urticaria (hives), rash, flushing, injection site reactions, nausea, constipation, or abdominal pain | atogepant (Qulipta), erenumab (Aimovig), fremanezumab (Ajovy), galcanezumab (Emgality), rimegepant sulfate (Nurtec ODT) |
| Selective serotonin reuptake inhibitors (SSRIs)16 | Decreases the amount of serotonin that goes back into the cell that released it | Preventive or acute | Headaches, nausea, trouble sleeping, dizziness, diarrhea, weakness and fatigue, anxiety, stomach upset, dry mouth, increased appetite | paroxetine (Brisdelle, Paxil, Pexeva), fluoxetine (Prozac), Fluvoxamine (Luvox), sertraline (Zoloft) |
Other therapies
Although drug treatments tend to become the go-to approach in managing migraine symptoms, therapies used in conjunction tend to provide another layer of protection and assurance.
Clinical trials have examined several types of therapies that have been used to treat vestibular migraine but are not limited to:
- psychometric physiotherapy
- cognitive behavioral therapy
- physical therapy/vestibular rehabilitation.
Psychometric physiotherapy
Psychometric physiotherapy is a type of rehabilitation therapy in which the client works with a physiotherapist in order to better manage their condition.17
Sessions typically follow a client-centered therapeutic approach where the patient takes control over their healing as the therapist creates an atmosphere of safety and non-judgment.
Cognitive Behavioral Therapy
Cognitive Behavioral Therapy, or CBT, has been an effective therapeutic approach that has been utilized across a breadth of topics in mental, physical, and emotional health. CBT combines both a cognitive and behavioral focus to develop healthy self-esteem, behaviors, personal coping skills, problem-solving, and regulation of emotions in the face of personal adversity.
Previous studies have cited CBT as an effective therapy to use simultaneously with drug modalities in the treatment of migraine.5
Both CBT and psychometric physiotherapy allow for honest, open forums between the therapist and client about the emotional struggles that come from managing migraine/vestibular migraine.
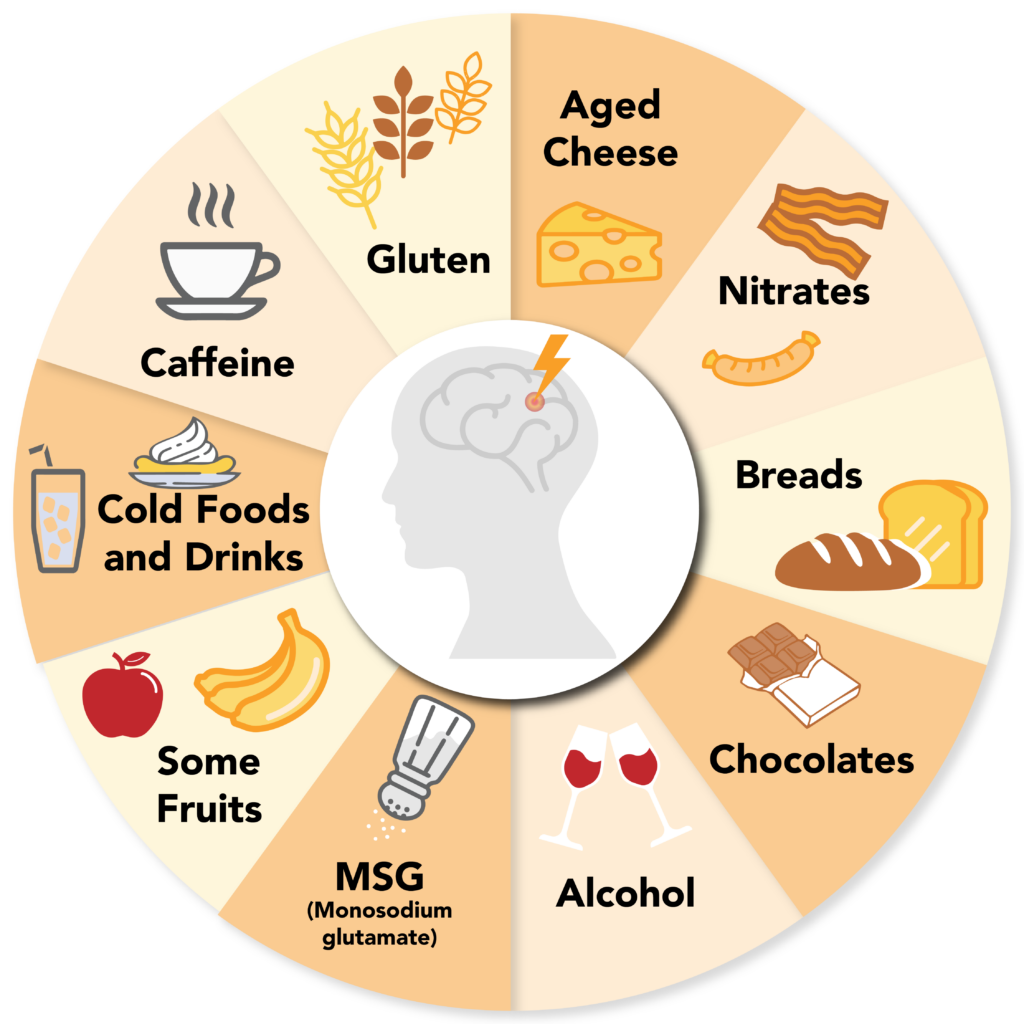
Vestibular rehabilitation
Vestibular rehabilitation, or vestibular rehabilitation therapy, on the other hand, demands more physical actions on the part of the patient. Vestibular rehabilitation is a type of physical therapy that specializes in treating or improving the symptoms that surround vestibular disorders, such as dizziness, vertigo, visual disturbances, and refining balance and posture.18
This type of therapy usually is administered by a physical therapist by referral from a physician. The outcomes of sessions are dependent on the type of vestibular symptoms present. Thus, the length and overall prognosis of the sessions could span months to years in some individuals. Similar to traditional physical therapy, the therapist utilizes different procedures to address the patient’s concerns and will require the patient to practice building their new skills with at-home exercises. Examples of the typical procedures in treating vestibular symptoms include but are not limited:
- lempert maneuver
- gaze stabilization exercises
- otolith repositioning maneuvers18
Most people don’t consider physical therapy when trying to find a viable solution to abating their vestibular symptoms. Dr. Teixido elaborates further on the purpose and benefits of incorporating physical therapy into a vestibular migraine treatment plan:5
Aside from rehabilitation, medication, and therapeutic approaches, there are more cost-effective treatment options for vestibular migraine patients to access to decrease the number of episodes and severity of their symptoms.
Exercise
If the sage old advice of partaking in exercise isn’t ringing a dead, broken bell, it’s only because clinical data has proven its whole body benefits. In terms of neurobiology, exercise has been proven to desensitize the brain to certain stimuli.2 While it may seem counterintuitive for vestibular migraine patients to engage in movement as a part of migraine management, in fact, engaging in moderate to high-impact exercises should not be discounted. Exercises such as jogging, running, cycling, hiking, playing various team sports, and many others are commonly cited as triggers in those with vestibular migraine, and, especially among those who are also diagnosed with exercise-induced and/or heat-induced migraine. However, the benefits of engaging in this level of exercise far outweigh the cons. Movement can release endorphin-inducing benefits.
Popular, low-impact exercises to consider are yoga, Tai Chi, walking, and vestibular therapy.2 It has been noted that people who suffer from vestibular migraine may find it difficult to engage in yoga or pilates due to certain head movements.
Adriane Dellorco also has some advice about how to avoid triggering a vestibular attack during an exercise routine:10
Experts have noted that there are ways to abate the negative side effects of exercise, specific for migraine patients.
These techniques include but are not limited to:
- Performing warm-up exercises before engaging in moderate to high-impact activities.
- Scheduling exercise routines at cool points in the day.
- Exercising in shaded areas.
- Staying hydrated before and after exercising.
- Being mindful of your limits; pushing oneself with caution.
- Consulting with a physician to determine whether or not moderate to high-impact aerobic exercises will be beneficial.
Neuroplasticity training
In the same vein as vestibular therapy, there are talks among experts about whether or not neuroplasticity training could provide some additional support in improving patient quality of life. Neuroplasticity refers to the brain’s potential to grow, change, and rewire itself. For example, engaging in everyday tasks such as learning a new skill, seeking positive social interactions, participating in novel experiences, taking up an exercise routine, and practicing mindfulness are all examples of neuroplasticity as they help establish and build neural connections.
Clinical neuroplasticity training is different. It shares some overlap with vestibular therapy; however, its aim is to help patients at the cellular level by creating and restructuring neuronal connections to improve cognitive functioning, decrease chronic pain signals, and help improve neural pathways to achieve better mental and physical health. This type of therapy can also help decrease sensitivity to vestibular stimuli that could contribute to dizziness and balance problems.2 The targeted area of study in the brain is the limbic system, and more specifically, the amygdala. The idea is that the limbic system is involved in the “fight or flight” response to certain emotional stimuli and past negative experiences can create, within the pathway, overactive neural signals of chronic pain.19 The goal of this therapy is then to rewire, at the neural level, how the limbic system responds to negative triggers to decrease chronic pain levels.
Other methods of treatment
There are new treatments developing outside the realm of drugs and therapy. A prime example of this are electronic neuromodulation devices. There are currently four neuromodulating devices on the market:
Neuromodulating devices
E-TNS– an external trigeminal nerve stimulator (Cefaly)
nVNS – a noninvasive vagal nerve stimulator (Gammacore)
sTMS– a single-pulse transcranial magnetic stimulator (sTMS mini)
REN – a remote electrical neuromodulator (Nerivio)20
These devices are great options for patients who have exhausted medication options or who show sensitivity to certain medications. Each of these devices shows promise and works to stimulate different cranial nerves to block pain signals.
Outlook/Prognosis
Although living with a chronic disease as debilitating as migraine can seem like a lifelong burden, there is a break in the storm clouds. The field of migraine research is an ever-changing landscape with many advancements being made every year. Studies are also being replicated to better answer the questions that plague researchers as well as patients. The path to understanding migraine, in all its tangled web of complexity, is being studied now more than ever. It’s truly a time to feel hopeful, especially for vestibular migraine patients.
Dr. Beh offers a ray of hope to those seeking an end to their debilitating symptoms.2
While finding a permanent solution to vestibular migraine, and chronic migraine in general, is still in development, it is reassuring to know that it might be on the horizon. There are many chronic and debilitating conditions, but none are as misunderstood and stigmatizing as chronic migraine, which the general consensus considers a “silent disease.” With every demographic being susceptible, it makes the name silent disease all the more disheartening. But, as always, the more awareness raised, the greater the quality of living for those who are waiting for the day they can finally rid themselves of their symptoms and bring order back into their lives.
Additional Resources
-
- Migraine Associated Vertigo Support Group (Facebook)
- Migraine Community Groups
- Move Against Migraine (Facebook)
- The Daily Migraine (Facebook)
- Headache Impact Test
- Migraine Disability Assessment Questionnaire (MIDAS)
- Coalition for Headache And Migraine Patients [CHAMP] (USA)
- American Migraine Foundation (USA)
- Association of Migraine Disorders (USA)
- National Headache Foundation (USA)
- Patient Advocate Foundation (USA)
- Work Accommodations for Migraine