An Introduction to Triptans
Triptans are a class of drugs specifically designed for the acute episodic treatment of migraine attacks. The first triptan, sumatriptan (Imitrex), was available for the abortive treatment of migraine in 1992, making triptans a well-established migraine treatment option today. Triptans are often one of the first drugs prescribed to individuals living with migraine. Today, there are seven different types of triptans that have emerged since the early 1990s.13
In an interview with Dr. Messoud Ashina, professor of neurology at the University of Copenhagen in Denmark, Paula Dumas of the Migraine World Summit asks about the 10-step treatment plan for migraine.2
Types of Triptans
Triptans are often where physicians’ playbooks start, as today they remain a first-line acute treatment for migraine. There are seven different types of Triptans: 5,13
- almotriptan (e.g., Axert)
- eletriptan (e.g., Relpax)
- naratriptan (e.g., Amerge)
- rizatriptan (e.g., Maxalt, Maxalt Mlt)
- sumatriptan (e.g., Imitrex, Onzetra Xsail, Tosymra, Zembrace, Symtouch, Sumavel DosePro)
- frovatriptan (e.g., Frova)
- zolmitriptan (e.g., Zomig, Zomig ZMT)
Did you know?
Did you know that for a migraine drug to be approved by the American Food and Drug Administration (FDA) it needs to have higher efficacy than a placebo in a double-blind study?
How Triptans Work
Triptans are serotonin reuptake inhibitors, also known as serotonin agonists and vasoconstrictors. This means triptans bind to serotonin receptor sites to both stabilize serotonin levels and inhibit the release of calcitonin gene-related peptide (CGRP). At the same time, triptans cause blood vessels to constrict (vasoconstriction).6 Triptans bind specifically to serotonin sites 5HT1B and 5HT1D, which changes the way pain is communicated by the cranial nerves to the brain.13 Through vasoconstriction, there is less blood flow to the brain, which is believed to reduce pressure placed on the blood vessels. It lessens the inflammatory pain experienced during a migraine attack.4
Dr. Deborah Friedman, neurologist, headache specialist, neuro-ophthalmologist and adjunct professor at Thomas Jefferson University, tells us at the 2022 Migraine World Summit, “In the early ’90s, the triptans came along. And the triptans were specifically designed to treat migraine; they targeted, directly, the serotonin receptors, and they changed people’s lives. So, you know, triptans and some of the ergotamines were the first targeted therapies specifically made for migraine.”2
If one triptan doesn’t work for you, another triptan might.
Each type of triptan has a slightly different effect on the body. For example, the half-life of frovatriptan is 26 hours compared with sumatriptan, which is 1-4 hours. Triptans have a greater than 50% efficacy rate for most people. Some people may respond to one triptan and not another, or find that one triptan works better than another. Deciding which triptan is best for you is determined by a discussion with your doctor. Your health profile, diagnosis, and personal medical history will be taken into account.2,5,13
Triptans can be taken orally, through a nasal spray, or via a subcutaneous injection. Nasal sprays and injections are well-suited for people who may experience nausea and vomiting with migraine attacks, making them unable to absorb oral medication in their system. Nasal spray and injections are also faster-acting, which makes them especially helpful for people who wake up with a migraine.
Triptan Dosage and Administration
Below are the seven triptans available for the acute treatment of migraine.6
| Triptan Type | Administration | Possible Side Effects7 |
| almotriptan (e.g., Axert) | oral/tablet | dizziness, drowsiness, nausea, sensations of tingling or warmth |
| eletriptan (e.g., Relpax) | oral/tablet | dizziness, drowsiness, nausea |
| naratriptan (e.g., Amerge) | oral/tablet | dizziness, drowsiness, nausea |
| rizatriptan (e.g., Maxalt, Maxalt Mlt) | oral/tablet | dizziness, drowsiness, nausea, sensations of tingling or warmth |
| sumatriptan (e.g., Imitrex) | oral/tablet (Imitrex), injection (e.g., Alsuma, Imitrex), nasal spray (e.g., Imitrex, Tosymra) or nasal powder (Onzetra) | dizziness, drowsiness, nausea, sensations of tingling or warmth |
frovatriptan (e.g., Frova) | oral/tablet | dizziness, drowsiness, nausea |
zolmitriptan (e.g., Zomig) | oral/tablet (Zomig) and nasal spray (Zomig Nasal Spray) | dizziness, drowsiness, nausea |
| Triptan Type | Contraindications (these are red flags in triptan use)7 | Max. Adult Daily Usage = 24 hours5,7,11 |
| almotriptan (e.g., Axert) | vascular conditions, such as: ischemic heart disease, stroke, peripheral vascular disease, uncontrolled hypertension | 25 mg., not to exceed 10 treatments or 250 mg./month |
| eletriptan (e.g., Relpax) | vascular conditions, such as: ischemic heart disease, stroke, peripheral vascular disease, uncontrolled hypertension | 80 mg., not to exceed 10 treatments or 800 mg./month |
| naratriptan (e.g., Amerge) | vascular conditions, such as: ischemic heart disease, stroke, peripheral vascular disease, uncontrolled hypertension | 5 mg., not to exceed 10 treatments or 50 mg./month |
| rizatriptan (e.g., Maxalt, Maxalt Mlt) | vascular conditions, such as: ischemic heart disease, stroke, peripheral vascular disease, uncontrolled hypertension | 30 mg., not to exceed 10 treatments or 300 mg./month |
| sumatriptan (e.g., Imitrex) | vascular conditions, such as: ischemic heart disease, stroke, peripheral vascular disease, uncontrolled hypertension | 200 mg. tablet 40 mg. nasal spray 12 mg. injection |
| frovatriptan (e.g., Frova) | vascular conditions, such as: ischemic heart disease, stroke, peripheral vascular disease, uncontrolled hypertension | 7.5 mg., not to exceed 75 mg./month |
| zolmatriptan (e.g., Zomig) | vascular conditions, such as: ischemic heart disease, stroke, peripheral vascular disease, uncontrolled hypertension | 10 mg. tablet or nasal spray |
In an interview with Dr. Messoud Ashina in 2022, Paula Dumas of the Migraine World Summit asks: “Is there any reason why everyone shouldn’t use a triptan, [or newer drugs such as a] ditan, or a gepant?”
Dr. Ashina replies,
“How is it possible that after 30 years of having triptans on the market … we still have a quite large number of patients who have never tried triptans, or who have tried only one triptan? And with the introduction of the new medications, such as gepants and ditans, we will be forced to try triptans because of the reimbursement rules. … That’s why the optimization of acute treatment should be something every neurologist and GP remembers.”8
Triptan Efficacy
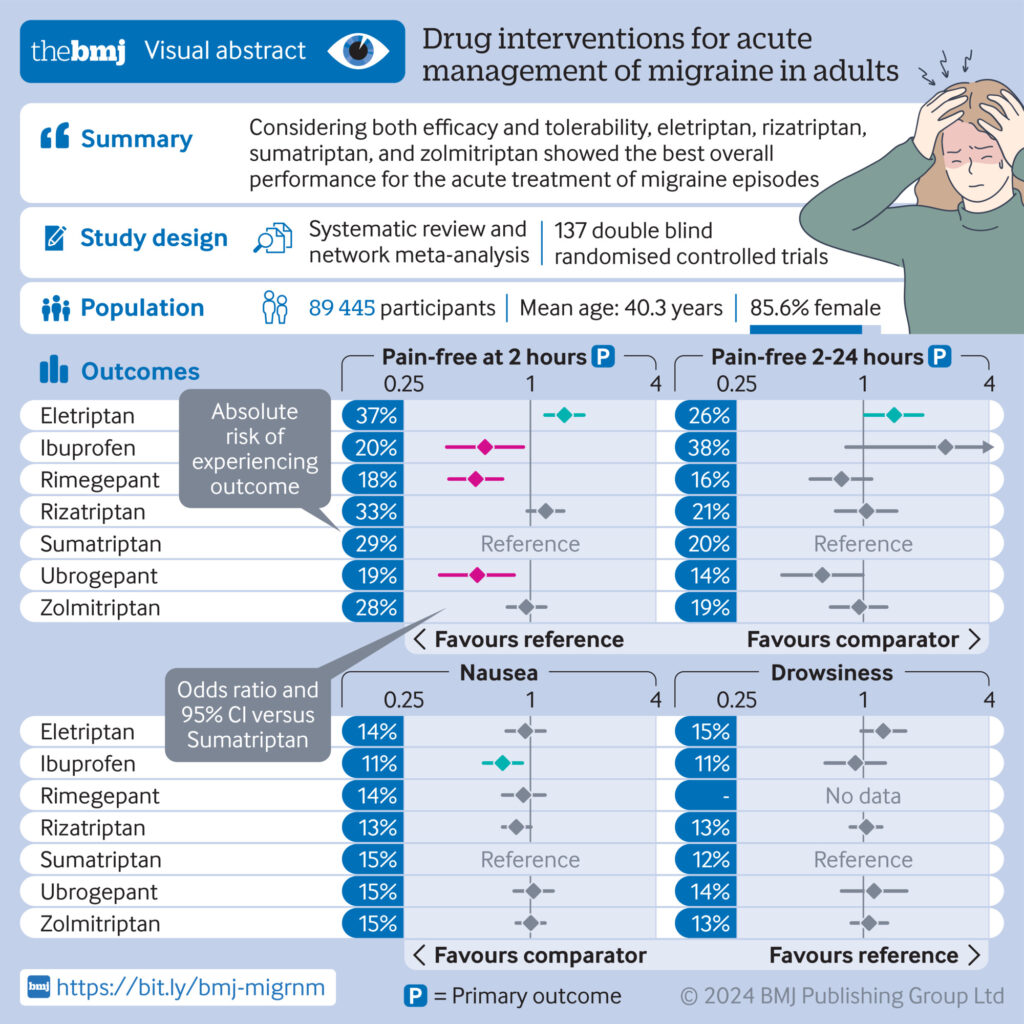
Published in September, 2024, a systematic review and network meta-analysis compared all licensed drug interventions for the acute treatment of migraine attacks in adults. Overall, eletriptan, rizatriptan, sumatriptan, and zolmitriptan had the best profiles. They also were found to work more effectively than newer drugs including lasmiditan, rimegepant, and ubrogepant.17
See the image below, from bmj.com, for more details on the comparisons.
Triptan Side Effects
Side effects of triptans include the following:18
- Chest Pain (rare)
- Dizziness
- Drowsiness, Fatigue
- Flushing
- Nausea
- Neck Pain
- Sweating
- Tingling, Numbness or a Pins and Needles Feeling in the Hands and Feet
- Weakness
Triptan Safety in Special Populations
People With Heart Conditions
Triptans are contraindicated, not considered safe, for people with heart conditions and vascular disease like high blood pressure, Raynaud’s, heart attack, stroke, etc. Dr. Gretchen Tietjen, professor emerita of neurology at the University of Toledo, provided insight on this in her interview on “Migraine Changes in Older Adults” during the 2023 Migraine World Summit.22
Dr. Tietjen says, “One of the things I think that has always vexed people the most, until hopefully recently, now that we have some new drugs that could replace it, but acute medications like the triptans cause vasoconstriction, which means any blood vessel in your body, which has this type of receptor on it — the serotonin receptor of a certain type — if you had that drug in your system, it could cause some — potentially it could cause some vasoconstriction of your coronary artery disease. Now, that is not common at all, but it’s not unheard of.”22
She adds, “That’s why with those drugs, once a person develops cardiac disease and has had a heart attack or has angina symptoms — which is sort of a warning for a heart attack — it’s thought, ‘do not use that medication anymore.’”22
Senior Citizens
Triptans are regularly prescribed to seniors without major vascular or cardiac concerns; however, more studies are needed on the 65+ population. Two recent studies suggest older adults using triptans for migraine may have low increased stroke risk. Still, the researchers of those studies advise, “Migraine treatment in the older population requires careful consideration of increased medical comorbidities.”
Children and Adolescents
Triptans are prescribed less often in children; ibuprofen is recommended for initial treatment for those under age 12.21 Rizatriptan is the only FDA-approved triptan for use for all children ages 6-17.20
In adolescents, sumatriptan/naproxen tablets, sumatriptan nasal spray, and rizatriptan or almotriptan oral-dissolving tablets are recommended for initial treatment. Abortive medications are more effective when used early after the onset of migraine in adolescents and adults.21
Pregnant Women
During the 2017 Migraine World Summit, Paula Dumas and Dr. Matthew Robbins, associate professor of neurology at Weill Cornell Medical College, New York-Presbyterian Hospital, discussed migraine treatment during pregnancy. In regard to triptans, he says, “The tradition has always been to avoid triptans in pregnancy because of the potential for birth defects or the potential to reduce blood flow through the placenta, but recent large studies and registry studies over a decade or more have not shown a major signal of elevated birth defects when compared to the general population, so there is a trend nowadays of using triptans on occasion in those who already have a track record for responding to them before their pregnancy, as long as it’s done in moderation.”19
Nursing Mothers
Dr. Robbins also shared advice on triptan use during breastfeeding. He says, “The general principle for breastfeeding is looking at the ratio of a medicine in milk to plasma, and every medicine has this known ratio, so those that have these lower ratios are safer than those that have the higher ratios, and it has to do with protein binding and other features.”
He adds, “So, for example, of all the triptan medications, eletriptan, which has the brand name Relpax, is probably the safest, because it’s cleared the least into breast milk. But also other considerations have to be taken into account; so, for example, if a woman is breastfeeding a baby who was born premature, and there are crucial concerns about neurological development of that baby, you might really avoid any medications that might impact alertness or awareness that could have deleterious consequences.”19
When to Use a Triptan
Triptans work best if taken at the first signs of a migraine attack, or within the first two hours of migraine onset. The earliest signs of a migraine attack include prodromal symptoms such as yawning, fatigue, irritability, and food cravings. At the first signs of a migraine attack, it is up to the individual to determine if they will choose a triptan to abort the migraine or use an NSAID, analgesic, or other treatment option.10
Did you know?
Did you know triptans work well with some over-the-counter medications, such as NSAIDS and acetaminophen?1
Combinations/Layering Strategies
Triptans, NSAIDS, and Analgesics
Triptans work well with some non-steroidal anti-inflammatory drugs (NSAIDs).1
Common over-the-counter NSAIDs include naproxen (e.g., Aleve) and ibuprofen (e.g., Advil, Motrin). Some triptans, such as sumatriptan, also come with naproxen added.1 Triptans also work well with acetaminophen (e.g., Tylenol, FeverAll), which is a common analgesic. Some people choose to use an NSAID and/or acetaminophen at the first signs of a migraine attack since:
a) Triptans are not to be used more than 10 times per month.
b) Not all migraine attacks may require a triptan.
If the migraine attack recedes, the individual may not need to use a triptan. If the attack does not recede within the first two hours of symptom onset, then a triptan is still available for use.
Triptans and Medication Overuse Headache (MOH)
Triptans should not be used more than 10 times per month. This makes triptans effective for the acute treatment of episodic migraine less than 10 days per month. Episodic migraine is defined as having less than 15 attacks per month.8
When triptans are overused, or overused in conjunction with NSAIDs or acetaminophen, people can develop a complication called medication overuse headache (MOH). MOH can present as a daily dull headache or a daily migraine. In most cases, reducing the use of the offending medication will reverse MOH. In some cases, MOH leads to chronic migraine. Chronic migraine is a condition defined as 15 or more headache days per month, with at least eight of those being migraine attacks, for at least three months.8,11
Often people living with migraine are continually searching for the best treatment option for them. If they have tried one triptan and it was not effective, or the side effects of the triptan were considerable, it may be helpful to try other triptans before moving to more expensive or invasive treatment options.
Paula Dumas of the Migraine World Summit asks: “People who might be at risk for medication overuse headache, or rebound: Are we finding that gepants are a better option for those folks?”
Dr. Dodick, director of the headache program at the Mayo Clinic in Arizona, responds:
“Yeah, that’s a great question. So, one of the key attributes of the gepants is that they may be the first, really the first, acute treatment for migraine that doesn’t cause medication overuse headache, or rebound. In fact — and maybe if you take a gepant every day, you actually drive the frequency down. So you’re going to see a medicine now that’s approved for acute treatment. … So people who have gotten into trouble before with rebound, from triptans, or opioids, or analgesics or whatever sort — these gepants, both in animals and now in humans, don’t seem to cause rebound or medication overuse headache.”8
Did you know?
Did you know that if none of the triptans provide effective relief for you, there are other new options available, such as ditans and gepants?
Triptans and Ditans
Ditans are a new class of drugs for the acute treatment of migraine. Ditans became available for use in the United States healthcare system in 2019. Both ditans and triptans work by blocking the release of CGRP, but unlike triptans, ditans do not dilate blood vessels. This makes ditans safer for people living with migraine and vascular diseases, such as cardiovascular disease, Raynaud’s syndrome, high blood pressure, diabetes, or stroke. Ditans are more expensive than triptans and are not as readily accessible in as many countries as triptans.10
Triptans and Gepants
Gepants are a new class of drugs for both the acute and preventive treatment of migraine attacks. This represents a recent breakthrough for migraine management. Gepants are CGRP antagonists that block CGRP receptor sites, but unlike triptans they do not constrict blood vessels or arteries. This makes gepants safe for people living with vascular diseases, such as cardiovascular conditions, Raynaud’s syndrome, high blood pressure, diabetes, or stroke. Gepants are more expensive than triptans and are not as readily accessible in as many healthcare systems worldwide as triptans.7
During their 2021 Migraine World Summit interview, Paula Dumas and Dr. David Dodick discuss geptans and how they differ from triptans.
Click here for their discussion
Dr. Dodick explains, “So gepants bind to that CGRP receptor on the trigeminal nerve and block the effect of CGRP. Triptans inhibit or suppress the release of it, whereas gepants block its ability to act because it gums up the receptor, if you will. That’s the difference. CGRP receptor antagonists, or gepants, bind to the blood vessel, but they dilate the blood vessel rather than constrict the blood vessel. So CGRP, when it binds to a blood vessel, dilates it.”11
Dumas says, “What I’m hearing you say is, they appear to be safer for people who have either heart issues or a family history of heart problems.”
Dr. Dodick: “They appear to be because they don’t constrict blood vessels. And so, now, of course, we use them in people who do have cardiovascular disease, and they appear to be safe … And they’re not contraindicated in people who have had heart disease or stroke, and we’ve been using them in those patients and seemingly safely. So they’re an option for patients who can’t take triptans because of this cardiovascular risk. And because they work differently, they don’t have the same side effect profile. So, the most common side effects seen with the gepants — and in a very small number of patients in clinical trials — some had a little bit of fatigue, and some had a little bit of nausea, but 95% of the patients had no side effects — as opposed to triptans, where they have a completely different side effect profile. So far, we have a class of medicine where if a patient doesn’t respond to a triptan, can’t take a triptan, or has side effects from a triptan, this may be a reasonable option. And I should say, there’s data that supports that they can be effective in people who have failed triptans.”
In the video below, Dr. Dodick discusses the incredible significance of these new treatment options, both for patients and practitioners.
Triptans and Botox
OnabotulinumtoxinA, Botox, is a neurotoxin designed to block nerve stimulation and relax muscles.7 Injections are given in the face, head, and neck. Botox is available for people living with chronic migraine. Unlike triptans, Botox was not specifically designed for migraine treatment and does not target CGRP or blood vessels. However, many people find it an effective treatment to help prevent acute migraine attacks. Botox is accessible in most countries and is more expensive than triptans.
Triptans and Opiods
Opioids are a broad class of drugs that enhance pleasure and block pain receptor sites in the brain. They are most commonly used following surgery and for the treatment of chronic pain conditions. Opioids are not recommended for the treatment of migraine due to their addictive nature.
Drug-to-Drug Interactions23
Triptans with MAOIs
The enzyme monoamine oxidase (MAO) in MAOI antidepressants breaks down some or all of the following four triptans: almotriptan, rizatriptan, sumatriptan, and zomitriptan. Eletriptan, frovatriptan, and naratriptan, however, are not broken down by MAOIs and, therefore, are better options for people with migraine on MAOIs.
Triptans with SSRIs and SNRIs
People on triptans and an SSRI (serotonin reuptake inhibitor antidepressant) or SNRI (serotonin norepinephrine inhibitor antidepressant) run the risk of developing serotonin syndrome, since triptans and these antidepressants each affect serotonin levels. The rare condition can cause confusion; changes in blood pressure; increased heart rate and sweating; and muscle changes like twitching, jerking, and clumsiness. While serotonin syndrome is rare, it’s good to know about it, so it can be recognized and treated should it occur.
Triptans with Ergots
No large studies have been conducted to evaluate the effect, so the exact narrowing process is unknown, but ergots may constrict arteries, and triptans are estimated to constrict normal heart arteries by up to 20%. To avoid potentially harmful blood vessel narrowing, triptans and ergots are not to be taken on the same day.
The Bottom Line
Triptans are a class of drugs used to acutely treat migraine attacks. There are seven different types of triptans, and each works a little differently. If one triptan doesn’t work well for a person’s migraine attacks or the side effects of the triptan are considerable, another triptan may be tried and found to work better. While shown to be highly effective when taken early during an attack, and often considered a first-line migraine treatment, triptans are not a good fit for everyone. Medication overuse headache, MOH, or a history of cardiovascular disease are two reasons why doctors may choose a different medication, such as a gepant or ditan, instead of a triptan.


