Understanding key medical terminology can be crucial for effective communication, diagnosis, and management of any disease or disorder. Getting a good handle on migraine and headache terminology, with all its complexities, can be especially helpful.
The following guide provides clear, concise definitions for common migraine and headache terms regularly discussed in our Migraine World Summit interviews with the world’s top headache specialists. Peruse this primer, and get a step ahead for the next Summit—and, ultimately, a step ahead in your care.
Types and Classifications of Migraine

| Migraine | This complex neurological disease is characterized by a severe headache accompanied by other symptoms such as:
Migraine attacks can be highly debilitating and significantly impact a person’s quality of life. To learn more, read our article on the various types of migraine, including silent migraine, or acephalgic migraine, vestibular migraine, etc. |
| Episodic Migraine | This refers to migraine that occurs on fewer than 15 headache days per month. |
| Chronic Migraine | Chronic migraine is diagnosed when a person experiences headache on 15 or more days per month, for at least three months, with at least eight of those days meeting the criteria for a migraine attack. This condition can be particularly debilitating and often requires comprehensive management strategies, as explained in this article on chronic migraine. |
| High-Frequency Episodic Migraine | This is when an individual has 10-14 migraine attacks per month. While not yet classified as chronic migraine, people with high-frequency episodic migraine are at an increased risk of progressing to chronic migraine. |
| Migraine with Aura | This is a subtype of migraine that includes transient neurological symptoms that typically precede, or sometimes accompany, the head pain. Aura symptoms may include: visual disturbances, numbness, weakness, and trouble with language. Aura symptoms usually last between 5 and 60 minutes. For more information, see our article on migraine with aura. |
| Status Migrainosus or Status Migraine | This is a severe migraine attack lasting longer than 72 hours. Unresponsive to standard acute treatments, it often requires urgent medical intervention. It may also be referred to as intractable migraine, which is often used more broadly in clinical settings to describe chronic migraine that is highly resistant to multiple treatments (see refractory migraine), while status migrainosus is the acute, prolonged attack. |
| Refractory Migraine | This term is used to describe migraine that has not adequately responded to multiple acute and preventive treatments, including oral medications, injectable therapies, and the use of neuromodulation devices. Managing refractory migraine often involves a multidisciplinary approach. |
| Hemiplegic Migraine | This is a rare and severe form of migraine with aura that includes temporary motor weakness or paralysis on one side of the body, mimicking stroke symptoms. It can be familial (FHM) or sporadic (SHM). |
Headache Classifications
Primary Headache | This is a headache that is not caused by another underlying medical condition. A few examples of primary headache are migraine, tension-type headache, and cluster headache. |
Secondary Headache | This headache is a symptom of another condition. These conditions can range from minor issues, like dehydration, to serious underlying causes, such as a brain tumor, aneurysm, or infection. “Red flag” symptoms typically prompt investigations to rule out secondary headaches. See our article on severe headache: when to worry. |
Stages of a Migraine Attack
A migraine attack typically progresses through four phases, though not everyone experiences all of them. This article explains the phases in depth.
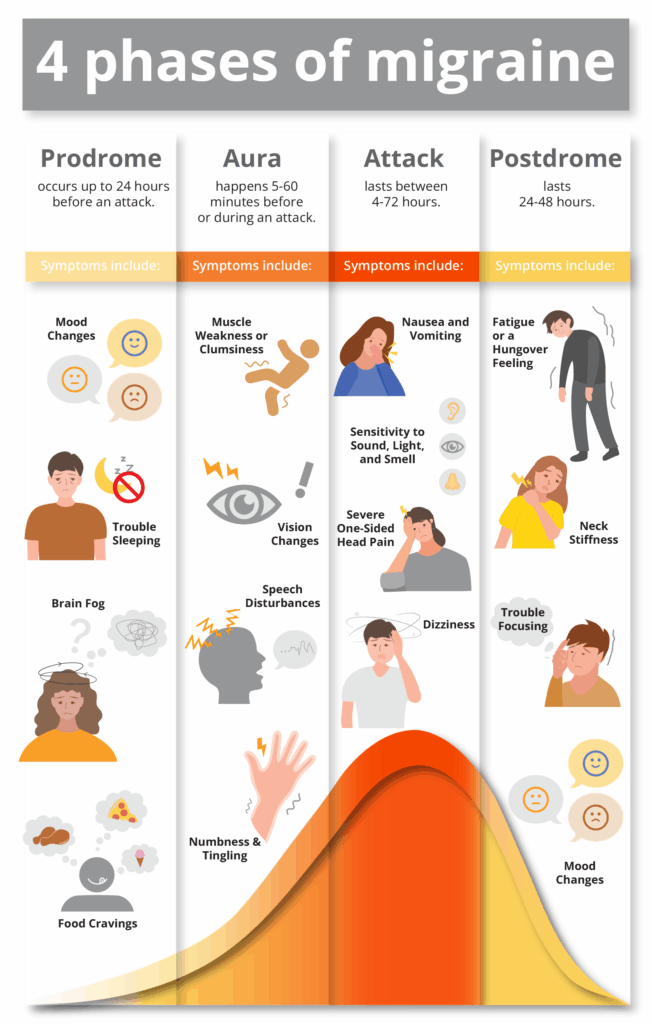
| Prodrome (Pre-headache) | This is the earliest phase, occurring hours or even days before the head pain begins. Symptoms can include fatigue, mood changes, neck stiffness, food cravings, frequent yawning, and increased urination. |
| Aura | This phase involves transient neurological symptoms that typically precede or accompany the head pain. Symptoms usually last 5 to 60 minutes and can include:
|
| Attack (Headache Phase/Ictal Phase) | This is often the most painful phase, characterized by head pain, often throbbing, and usually on one side of the head. It is commonly accompanied by light sensitivity, sound sensitivity, nausea, and vomiting. |
| Postdrome (Post-headache) | Following the attack phase, many individuals experience a “migraine hangover.” Symptoms can include fatigue, difficulty concentrating, mood changes, and neck stiffness. |
| Interictal | This phase refers to the period between migraine attacks when a person is not experiencing migraine headache. However, there may still be non-headache symptoms in between attacks such as brain fog, allodynia, or residual sensitivity to sound and light, for example. |
Specific Headache Types
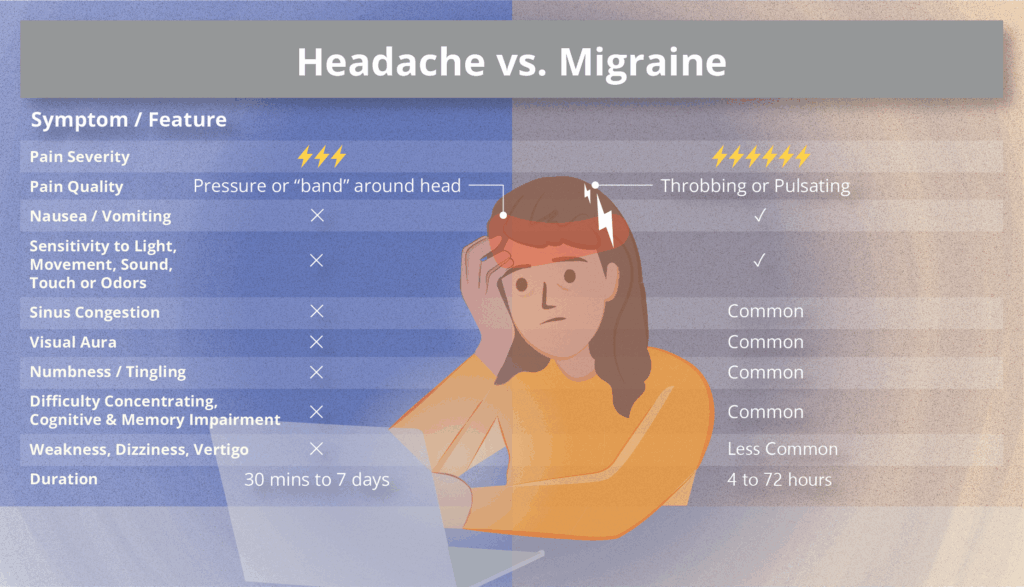
| Tension-type Headache | This is the most common type of headache, characterized by mild to moderate pain that feels like a tight band around the head. It typically lacks the associated symptoms of migraine, such as light and/or sound sensitivity, or nausea. |
| Cluster Headache | This severe primary headache disorder is characterized by excruciating pain, usually around one eye or temple. It is accompanied by autonomic symptoms such as tearing, nasal congestion, eyelid drooping, or facial sweating on the same side as the pain. Attacks occur in clusters, lasting weeks or months, followed by periods of remission. |
| New Daily Persistent Headache (NDPH) | This is a rare primary headache disorder characterized by a sudden onset of continuous daily headache that does not remit. The pain is present every day from onset and can have features of both migraine and tension-type headache. |
| Hemicrania Continua | This is a rare, chronic, unilateral headache that is continuous and fluctuating in intensity. It is characterized by autonomic features (like tearing or nasal congestion) on the affected side. It is notably responsive to indomethacin. |
| Idiopathic Intracranial Hypertension (IIH) | Characterized by increased pressure around the brain, this condition does not have an identifiable cause. Symptoms often include a daily headache, visual disturbances, and pulsatile tinnitus (hearing rhythmic sounds that match one’s heartbeat). |
| Medication Overuse Headache (MOH) | This chronic daily headache is caused by the overuse of acute headache medications. It often occurs when acute medications are taken frequently (e.g., more than 10-15 days per month), leading to a cycle of pain and medication use. It is sometimes referred to as medication adaptation headache or rebound headache. |
Migraine Treatments & Management

| Acute Treatment | This term is used for medications that are taken at the onset of a migraine attack to stop or reduce the severity of the pain and associated symptoms. Examples include: NSAIDs, triptans, gepants, and ditans. |
| Preventive Treatment | This includes medication or therapies taken regularly to reduce the frequency, duration, and severity of migraine attacks. These are typically considered for individuals with frequent or disabling migraine. Options may include: beta blockers, tricyclic antidepressants, anti-seizure drugs, Botox, CGRP inhibitors, and more. |
| Rescue Treatment | These are medications or therapies used when acute treatments have failed to provide relief, or for severe attacks that require stronger intervention. Sometimes these are provided in an emergency setting. |
Key Terms in Migraine Pathophysiology & Symptomatology
| Calcitonin Gene-Related Peptide (CGRP) | This neuropeptide is widely distributed in the nervous system, playing a significant role in migraine pathophysiology. During a migraine attack, CGRP is released from nerve endings, contributing to inflammation and pain signaling.
|
| Allodynia | A condition where a normally non-painful stimulus (like light touch, the brushing of hair, or wearing of glasses) is perceived as painful. It is a common symptom in migraine, indicating central sensitization (a chronic pain condition in which the central nervous system becomes hypersensitive, amplifying pain signals). |
| Aura | See “migraine with aura” above. |
| Brain Fog | A common cognitive symptom experienced by many people with migraine, characterized by difficulty with concentration, memory, and clear thinking. It can occur during any phase of a migraine attack, including the prodrome and postdrome phases. |
| Behavioral Treatment | Non-pharmacological therapies that teach individuals skills to manage migraine symptoms and reduce their impact. Examples include: cognitive behavioral therapy (CBT), biofeedback, and relaxation techniques. |
| Lifestyle Changes | Modifications to daily habits that can help manage migraine. These often include maintaining a consistent sleep schedule, regularly exercising, managing stress, identifying and avoiding triggers, and maintaining a healthy diet and adequate hydration. |
| Neuromodulation | This is the alteration of nerve activity through targeted delivery of electrical or chemical stimuli to specific neurological sites. In migraine, this often involves non-invasive devices that stimulate nerves like the trigeminal or vagus nerve to reduce pain and frequency. |
| Nonsteroidal Anti-inflammatory Drugs (NSAIDs) | A class of medications used to reduce pain, fever, and inflammation. Common over-the-counter (OTC) NSAIDs include ibuprofen and naproxen, often used for acute migraine relief. |
| Trigeminal Nerve | This is a cranial nerve that provides sensory input from the face and controls the muscles used for chewing (i.e., forehead, cheeks, and jaw). |
| Phonophobia | This is increased sensitivity to sound, a common symptom during a migraine attack. |
| Photophobia | This is increased sensitivity to light, a hallmark symptom of migraine, where even normal light levels can be painful or irritating. |
| Vagus Nerve | A cranial nerve that regulates involuntary bodily functions (i.e., heart rate, digestion, and breathing) and connects the brain to many organs, making it a major part of the parasympathetic (“rest and digest”) system. |
While it’s not exhaustive, familiarizing yourself with this list of key terms is an important step in understanding migraine disease. This knowledge can enhance communication with your healthcare providers and contribute to more informed discussions about your care. We encourage you to continue learning through our expert interviews, articles, and additional resources available on the Migraine World Summit website. Make sure to save the date for the next free Migraine World Summit: March 11-18, 2026!


