- Acute Medication for Migraine Headache
- Achieving the Most Effective Acute Treatment
- Different Types of Acute Migraine Medication
- How to Know What Acute Medication to Take and When
- How to Avoid Medication Overuse Headache (MOH)
- Preventive Medication for Migraine
- When to Start Using Preventive Medication for Migraine
- Tips to Find Your Most Effective Migraine Prevention
- Different Types of Preventive Migraine Medication
- Neuromodulation Devices for Migraine
- How to Find the Right Migraine Treatment for You
- Summary: Medication for Migraine Headaches
The landscape of medical treatment for migraine has evolved considerably over the years. It now offers a variety of medications to help alleviate acute attacks and prevent them in the future.
In this article you will learn more about the numerous medications offered to people with migraine today. It should allow you to easily prepare for your next doctor’s appointment, armed with knowledge.
Acute Medication for Migraine Headache
When you are experiencing a migraine attack, acute medication can be taken to stop or minimize the intensity and duration of the pain as well as other migraine symptoms.
Acute medication for migraine includes a range of options, from simple pain relievers and nonsteroidal anti-inflammatory drugs (NSAIDs) used to treat pain in general, to triptans and gepants, which are specially developed to treat migraine.1
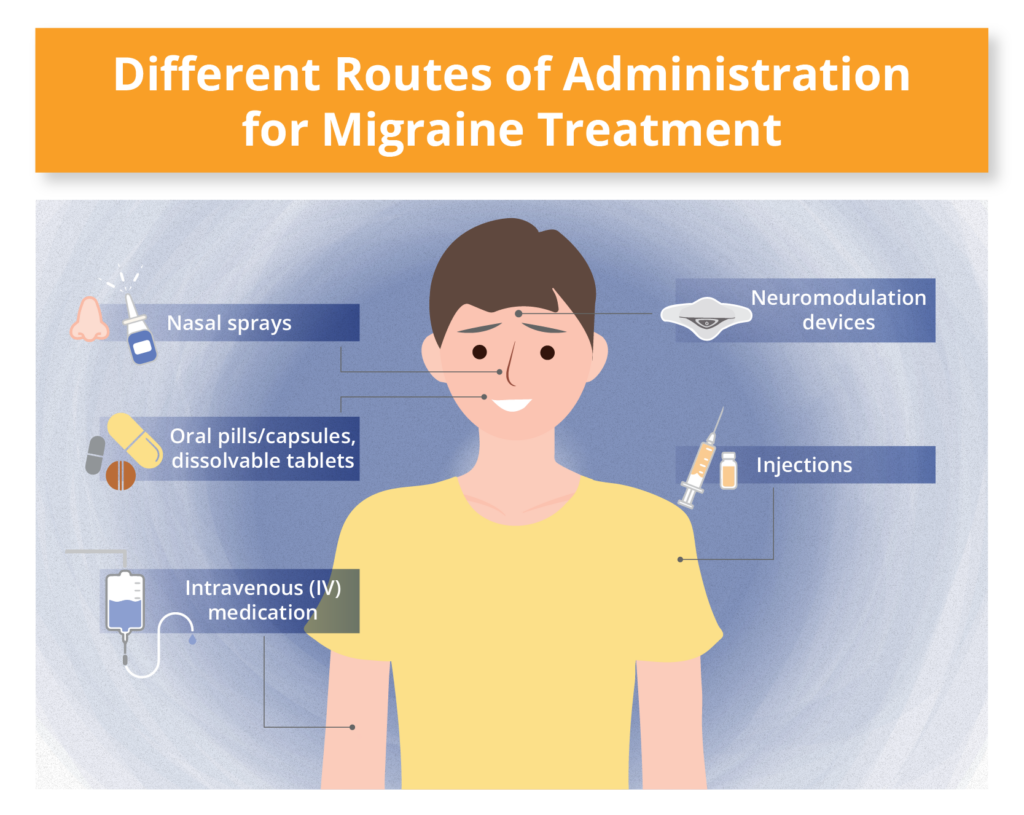
Acute medications are available in various forms, including oral pills, dissolvable tablets, nasal sprays, and injections. If you tend to vomit during migraine attacks, using nasal sprays or injections can help ensure that the medication remains in your system.
Achieving the Most Effective Acute Treatment
Most people who experience migraine attacks should consider acute medication. When effective, acute medication can significantly relieve attacks in either severity or duration, or both.
For the best possible effect, you should take your acute medication at the first sign of a migraine attack. Dr. Andrew Charles says that there have been multiple studies showing that treatment when pain is mild is beneficial.
“If you treat your migraine attacks when the pain is mild, studies show that there is a greater chance of reaching a pain-free endpoint, or pain relief within a certain period of time. In addition, the chance that an attack will recur is actually reduced,” says Dr. Charles.
Delays in taking acute medication can lead to increased pain, greater disability, and a more significant impact from the headache. The benchmark of an effective acute treatment is “back to function” within two hours of treatment.
In many cases, a combination of medications may be necessary to achieve adequate relief. However, do not mix medications on your own; these must be prescribed by your doctor.
When experiencing frequent migraine attacks, it can be challenging to avoid overusing acute medications. Using various types of medication, like over-the-counter pain relievers or triptans combined with NSAIDs for 10 days or more each month, can lead to medication overuse headache (MOH),2 also known as rebound headache. This can result in even more frequent migraine attacks and increased pain. You can read more about medication overuse headache and how to avoid it below.
Consider keeping a migraine diary to track your migraine attacks, what medication you use and its effects. There are several apps available for this purpose that you can download and easily access from your phone.
Different Types of Acute Migraine Medication
There are several different types of acute medication for migraine attacks. These include:
- ditans
- pain relievers (analgesics)
- NSAIDs
- triptans
- ergotamine
- gepants
First-Line Acute Treatments for Migraine
If you are experiencing mild to moderate migraine attacks, first-line acute treatment includes: pain relievers (analgesics). For example:10
- aspirin (Bayer)
- acetaminophen (Tylenol)
- NSAIDs including ibuprofen (Advil)
If you are experiencing moderate to severe migraine attacks, first-line acute treatment includes:10
- Triptans, including:
- sumatriptan (Imitrex) — this is the triptan commonly prescribed before trying others.
- zolmitriptan (Zomig)
- eletriptan (Relpax)
- rizatriptan (Maxalt)
- almotriptan (Axert)
- frovatriptan (Frova)
- naratriptan (Amerge)
It may take awhile to find a medication that is effective and well tolerated. Up to three different triptans may be tried via various routes of administration before physicians will look to another class of drugs, including gepants and ditans.10 Gepants and ditans are also prescribed to individuals who are unable to take triptans since these newer drugs don’t constrict blood vessels.10
- Gepants (CGRP small-molecule receptor antagonists), including:
- rimegepant (Nurtec ODT, Vydura)
- ubrogepant (Ubrelvy)
- zavegepant (Zaczpret)
- Ditans (selective 5HT1F receptor agonists) such as lasmiditan (Reyvow)
A New Drug on the Horizon
In January 2025 the FDA approved a new acute medication for migraine called Symbravo. Symbravo combines rizatriptan, a fast-acting triptan, and meloxicam, a long-lasting NSAID. It is designed to effectively relieve the most severe migraine symptoms quickly and maintain relief for a longer duration.12
Other Medications Available for the Acute Treatment of Migraine
Additional prescribed medications include ergotamine derivatives, such as dihydroergotamine (DHE). Many physicians also recommend treating migraine attacks with neuromodulation devices such as CEFALY and Nerivio (more on these below).
Also, if you experience nausea during your attacks, anti-nausea medication (antiemetics) can not only keep the acute medicine you take in your system but also enhance the absorption of it.
“Once people start getting nauseated, they’re much harder to treat. And we know that the gut is not working well in general during a migraine, even without nausea. Once people start getting nauseated, the likelihood of being able to swallow a pill, have it dissolved, have it be absorbed, and be effective, goes way down.”
Over-the counter (non-prescription) options in anti-nausea medication include dimenhydrinate (Dramamine) and diphenhydramine (Benadryl). Prescription antiemetics include metoclopramide (Reglan) and ondansetron (Zofran).
How to Know What Acute Medication to Take and When
According to Dr. Friedman, people living with migraine often have different kinds of attacks. Treatments should not only be tailored to each individual patient, but also to their specific type(s) of attacks.
“Share with your doctor the typical timeframe of a migraine attack, from when you first become aware of an attack, to then when the pain starts. How long does it take for your medication to work? Does the headache come back? What percentage of the time is your acute medication effective? This information may help you to get a better acute treatment plan,” Dr. Friedman explains.
How to Avoid Medication Overuse Headache (MOH)
Medication overuse headache (MOH) is a type of headache that occurs from using too much medication for an existing headache disorder, like migraine, and is common among individuals with 15 or more headache days per month.3 Medication overuse headache can occur when using various types of medication, like over-the-counter pain relievers or triptans combined with NSAIDs, for 10 days or more each month.4
Adding preventive methods to reduce headache frequency is important to prevent medication overuse headache. Another strategy to avoid medication overuse headache is to use gepants for preventive and/or acute treatment. Gepants have not been shown to contribute to medication overuse headache unlike other acute treatments.5
Preventive Medication for Migraine
The primary goal of preventive medication for migraine is to lessen the impact of the condition by reducing either the frequency or severity of migraine attacks — or both.
Preventive medication includes a range of options. These include antidepressants, beta blockers, calcium channel blockers, anti-seizure medications and Botox. There are also preventive medications developed especially for migraine, such as Calcitonin Gene Related Peptides (CGRP) monoclonal antibodies.
The medication comes in various forms, including oral pills, injections, and intravenous (IV) drugs. Successful preventive treatment for migraines is measured by its ability to reduce the disease burden and improve quality of life.
When to Start Using Preventive Medication for Migraine
Effective preventive migraine treatment starts with an accurate diagnosis, which may involve ruling out other potential causes of your symptoms. Whether or not you should take preventive medication depends on the number of migraine attacks you experience per month and how much they affect your daily life.
Practitioners suggest starting migraine preventive drug therapy when one or more of the following conditions is present:11
- You have more than three migraine attacks or at least eight headache days in one month.
- You have severe, debilitating headache attacks despite acute treatment.
- You have contraindications to acute medication or can’t tolerate its side effects.
- You have medication overuse headache.
- You have hemiplegic migraine, basilar migraine, or migraine with prolonged aura.
- You prefer to go on a preventive treatment.
Tips to Find Your Most Effective Migraine Prevention
- Don’t get discouraged if the first medication you try doesn’t have the desired effect. Finding a preventive medication that works for you may require some trial and error.
- Different preventive medications can complement each other, and you might need to use more than one.
- Keep a migraine diary to track your attacks, symptoms, and the effects of treatments.
- An effective preventive treatment is typically defined by a 50% reduction in the frequency or severity of attacks.
- If your doctor tells you they’ve tried everything or run out of options, it may be time to consider another doctor. There are many options and strategies to consider for someone who knows how to treat patients with migraine disorder.
Different Types of Preventive Migraine Medication
First-Line Treatments for Migraine Prevention
Options include:
- Anti-seizure medication (anticonvulsants), including divalproex (Depakote) and topiramate (Topamax)
- Blood pressure lowering medication, including beta blockers, such as propranolol (Hemangeol); also, calcium channel blockers, such as verapamil (Verelan)
Other Approved Treatments for Migraine Prevention9
- Antidepressants, such as amitriptyline (Elavil)
- Gepants, including rimegepant (Nurtec ODT) and atogepant (Qulipta)
- Calcitonin Gene Related Peptides (CGRP) monoclonal antibodies (mAbs), for example: erenumab (Aimovig), galcanezumab (Emgality), fremanezumab (Ajovy), and eptinezumab (Vyepti)
- OnabotuliniumtoxinA (Botox)
Due to comorbidities, other conditions you may have in addition to migraine, certain preventive medications may be better than others for you.9 For instance, calcium channel blockers may be preferred if you have dizziness or vertigo. If you have insomnia and/or depression, a tricyclic antidepressant may be chosen for you.
Neuromodulation Devices for Migraine
How Neuromodulation Devices Work
Neuromodulation devices, sometimes referred to as nerve stimulation devices or neurostimulation devices, modulate the activity of different nerves such as the occipital nerve, trigeminal nerve, vagus nerve, and the supraorbital and supratrochlear nerves in the forehead. Some neuromodulation devices are used for preventive treatment, some for acute treatment, and some have both options. These devices typically require a prescription.
When to Try Neuromodulation Devices
- If you experience side effects from medication (Neuromodulation devices have limited side effects because they are not absorbed in the body.)
- If you are in need of using acute medication more than 10 days a month
- If you are under 18 (Some neuromodulation devices are approved for adolescents.)
Food and Drug Administration (FDA)-Approved Neuromodulation Devices for Migraine:8
How to Find the Right Migraine Treatment for You
If you are living with migraine and it is negatively impacting your life, it is recommended that you consult a headache specialist or a neurologist. You may experience difficulty in finding or getting in to see a headache specialist, as they are in short supply. Keep in mind that neurologists aren’t necessarily headache specialists, but they tend to treat a lot of patients with migraine.
Ensuring that your treatment is specifically tailored to address both acute attacks and preventive care is crucial. Various types of medications, both acute and preventive, work well together. Consider keeping a migraine journal to track the effects of different medications.
Additionally, consider non-drug therapies such as neuromodulation devices, chiropractic care, cognitive behavioral therapy (CBT), and lifestyle changes like regular exercise and consistent sleep routines.
Supplements to Consider
Supplements are another class of treatment that often comes up when talking about migraine.
Dr. Alexander Mauskop, director and founder of the New York Headache Center, and a board-certified neurologist and headache specialist, explains which supplements he would typically recommend for those living with migraine.
“If we don’t have any blood work to help us determine what supplements to use, we would first recommend magnesium because it has the most scientific evidence, and about 50% of people are deficient in magnesium. Second, the most proven supplement would be coenzyme Q10. We have a very large study looking at 1,550 people with migraine, and fully one third is deficient in CoQ10. My next recommendation would be a vitamin B2 — riboflavin. And then we also recommend herbal products such as feverfew. Another herbal supplement that I recommend is boswellia — frankincense.”
Improvement: What to Expect
For those living with frequent migraine attacks, any form of relief, whether small or significant, is greatly appreciated. However, according to Dr. Stewart J. Tepper, professor of neurology, people often settle for less than they should.
“I’m never satisfied until people are really not having any disability or impact from their migraines, and their function across all aspects of their life is back to normal,” says Dr. Tepper.
“If somebody has a very good response to a subcutaneous monoclonal antibody, but is still having a migraine attack or two per week, where previously they might have had 20 headache days in a month, it’s a pretty dramatic improvement for that person. But it may not be as good as they can get.”
Dr. Tepper suggests multiple ways to get an even greater drop in headache days, and improvement in quality of life.
“One way is to move from a subcutaneous injection of a monoclonal antibody once a month to an intravenous monoclonal antibody, and even move to the highest dose of that intravenous monoclonal antibody. Another option is to add onabotulinumtoxinA, or Botox. Sometimes the combination of the two will have an additive, or a synergistic effect,” says Dr. Tepper. He adds, “We can also consider a switch to the daily or every-other-day oral medications and combining gepants. All of these offer opportunities for people to do even better.”
Summary: Medication for Migraine Headaches
Medication for migraine headaches includes both acute and preventive medication. Most people with migraine should consider acute medication to effectively stop migraine attacks.
If you are experiencing migraine attacks four or more days per month, you can talk to your doctor about preventive treatment. If you are severely burdened by your migraine attacks, two a month is enough to consider preventive medication. See the full list of recommendations under the section When to Start Using Preventive Medications for Migraine.
It’s important to use a migraine diary to track migraine attacks, symptoms, and the effects of treatments used. Above all, remember the process takes time. Finding the right treatment, both acute and preventive, is often a process of trial and error. Don’t lose faith that there is treatment out there that will be able to help you.


